Introduction
Point of Care Ultrasound (PoCUS) is the use of portable ultrasonography to answer specific, focused clinical questions at the bedside. It is an extension of both our clinical acumen and physical exam.
The most common initial test for the dyspneic patient is chest x-ray. Recently, growing evidence has shown that PoCUS can reliably detect interstitial edema or thickening with equal, if not better, sensitivity than CXR. While CT scanning provides the best test characteristics, it is impractical and comes with the cost of significant radiation.
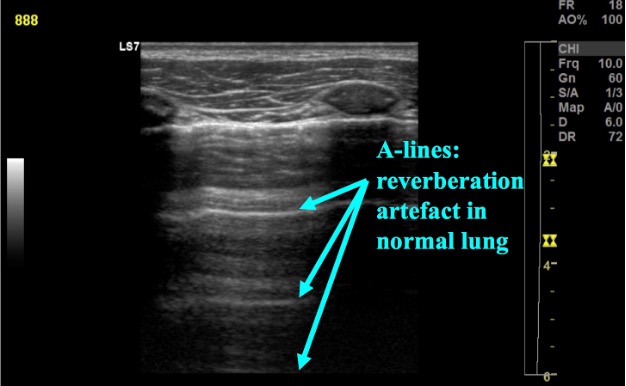
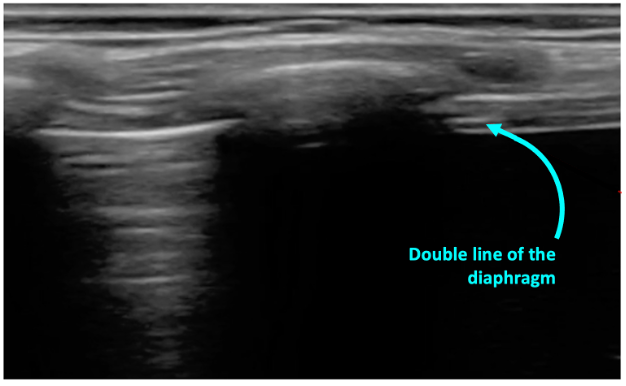
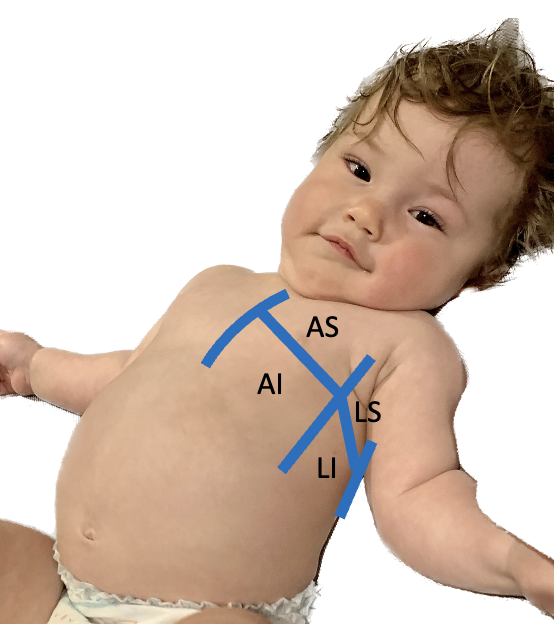
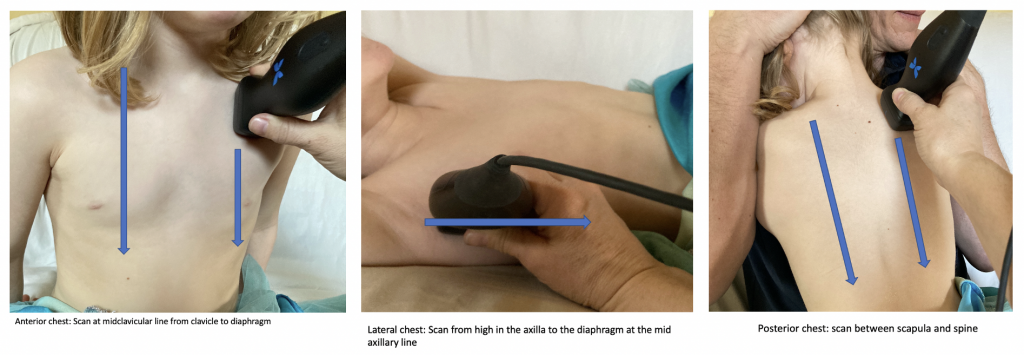
Ultrasound images of normal lung show predictable artifacts. These artifacts are disturbed in disease states and can be readily differentiated by ultrasound.
Why Ultrasound?
Traditionally, it was the thought was that ultrasound would not be a useful modality for investigating lung pathology because air scatters ultrasound waves. However, lung pathology (i.e. viral pneumonia/pneumonitis, cardiogenic pulmonary edema, contusion, pulmonary fibrosis, ARDS) will often lead to edema and fluid accumulation in the intersitium and alveoli. If this fluid or thickening reaches the pleural line these pathologies can be seen on ultrasound. This is the case in most patients, particularly children who have smaller lungs. This is supported by an ever-growing body of evidence.
International evidence-based guidelines have been published which support the use of point-of-care lung ultrasound in investigating various pulmonary pathologies, including interstitial disease [1]. In fact, LUS far outperforms radiography in the detection of interstitial diseases including viral pneumonia/pneumonitis, pulmonary edema, and pulmonary fibrosis [1,2]. In COVID-19 patients, LUS far outperformed conventional radiography, performing nearly as well as CT while decreasing radiation exposure and patient movement within hospital [3]. A recent meta-analysis looking at the test characteristics of LUS for pulmonary edema found a pooled sensitivity of 94% and specificity of 92% [4]. The test characteristics of LUS are superior to that of CXR in the diagnosis of acute pulmonary edema with the sensitivity of CXR ranging from 14-68% and specificity of 53-96% [5-7]. Also appealing, LUS is easier to interpret than CXR and the inter-reader reliability is consistently higher as well [8]. While these are adult studies and the test characteristics need to be studied in children, it is well proven that LUS performs at least as well in the pediatric population.
Logistically, a typical bedside ultrasound looking for pulmonary edema will take less than 5 minutes [9]. While system implications have not been studied for those with interstitial syndromes, a recent RCT studying the use of PoCUS in the diagnosis of pneumonia showed a 30-60% reduction in the use of CXRs, as well as significantly shorted ED length of stay in those patients’ receiving ultrasound vs. CXR [10]. Similar benefits could be expected in those with interstitial syndromes.