Indications
- Refusal to weight bear
- Limp
- Painful joint
- Swollen joint
Equipment
- Ultrasound machine
- Linear array probe (the curvilinear may be required for deep joins such as the hip in larger patients)
- Ultrasound gel
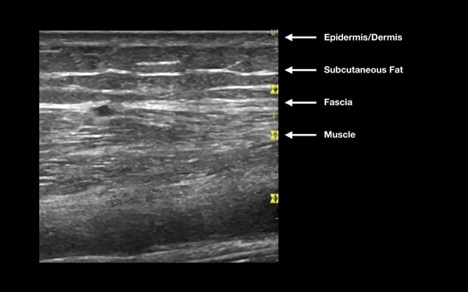
Normal skin and soft tissue have many layers (Figure 1). The most superficial structures are the epidermis and dermis, which appear as if one hyperechoic structure. Deep to this, you will find subcutaneous fat, which is hypoechoic and globular. Blood vessels, nerves and lymph nodes are found within the hypodermis, and are varying in their echogenicity. Deep to these structures, the muscle is found beneath a hyperechoic layer of fascia. Muscle is seen as highly organized hypoechoic and striated fibers.
Figure 1: Anatomy of normal skin
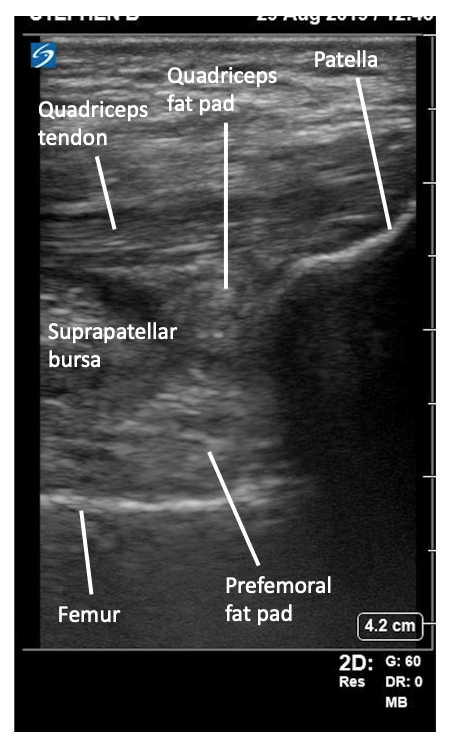
Tendons are visualized as hypoechoic fibrillar organized structures, whereas fat pads are also hypoechoic, but are more homogenous in their appearance (Figure 2). Finally, smooth hyperechoic bone cortex may be seen as the deepest layer.
Figure 2: Anatomy of a normal joint

In order to facilitate comparing an affected joint with the contralateral side, it can be useful to use the dual screen function on the ultrasound machine.
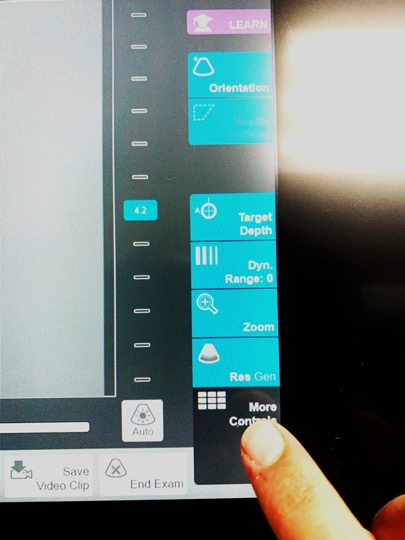 Figure 3a: Choose “more controls”
Figure 3a: Choose “more controls”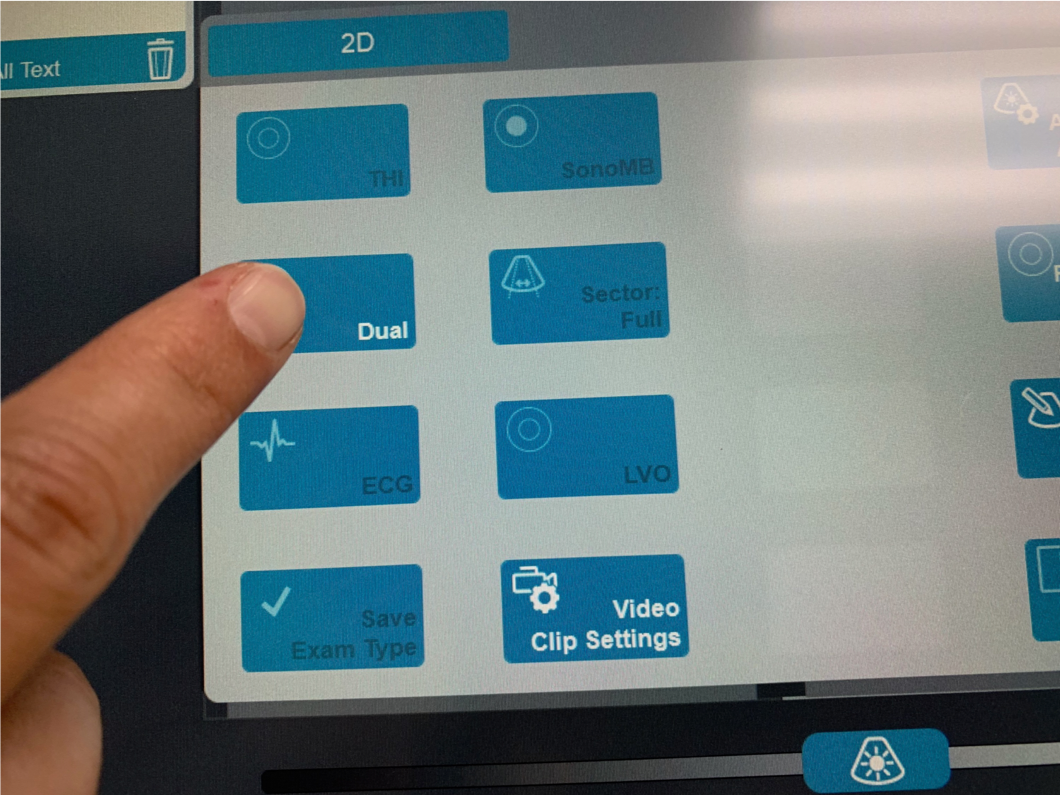 Figure 3b: Choose “dual”
Figure 3b: Choose “dual”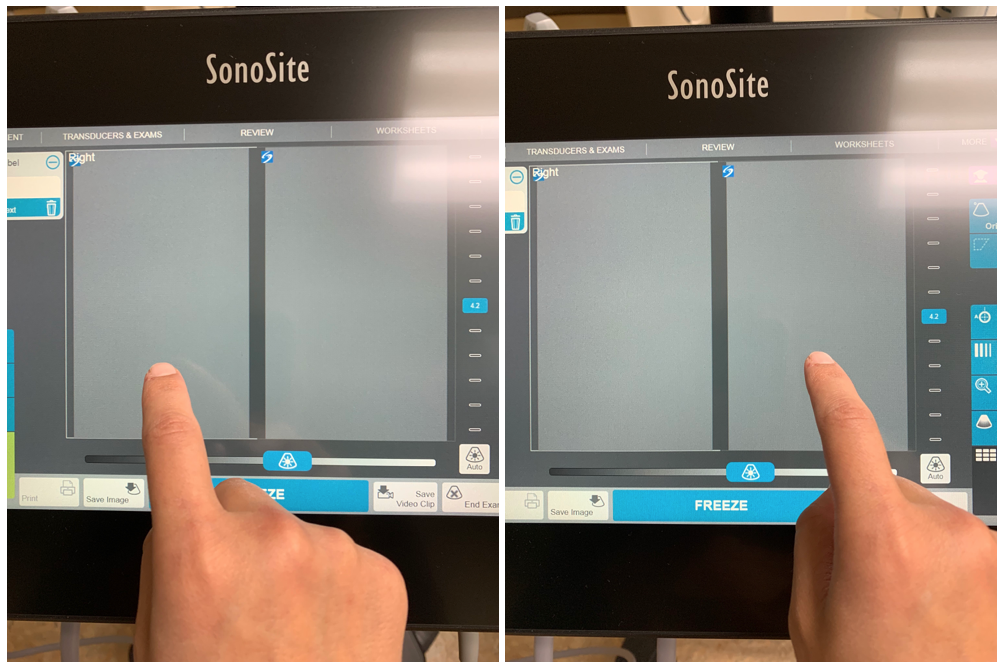 Figure 3c: Toggle between screens by touching the desired side
Figure 3c: Toggle between screens by touching the desired side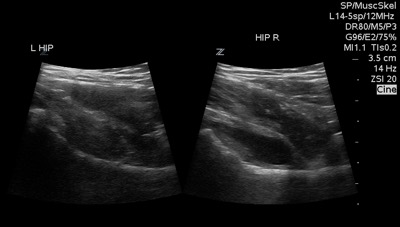 Figure 3d: Dual screen example
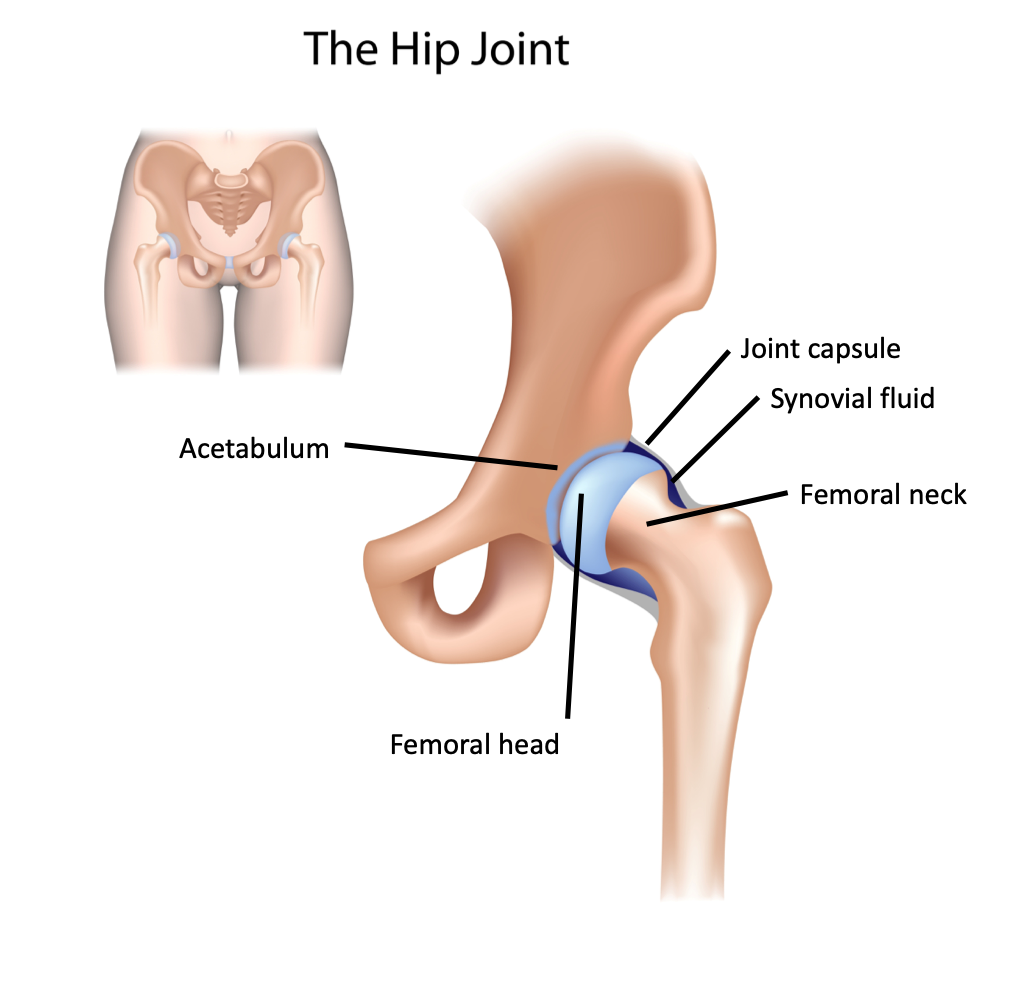
Figure 3d: Dual screen exampleThe hip joint is a ball and socket joint, comprised of the femoral head and neck and the acetabulum (made up of the ischium, pubis and ilium). The joint capsule surrounds these structures and contains synovial fluid (Figure 4).
Figure 4: Anatomy of the hip joint
Superficial to the bony structures, we find the musculature of the pelvis and the hip. Those that are relevant to us for the purpose of scanning for hip effusions include the iliopsoas, quadriceps and sartorius. These muscles are found superficial to the joint (Figure 5).
Figure 5: Hip musculature
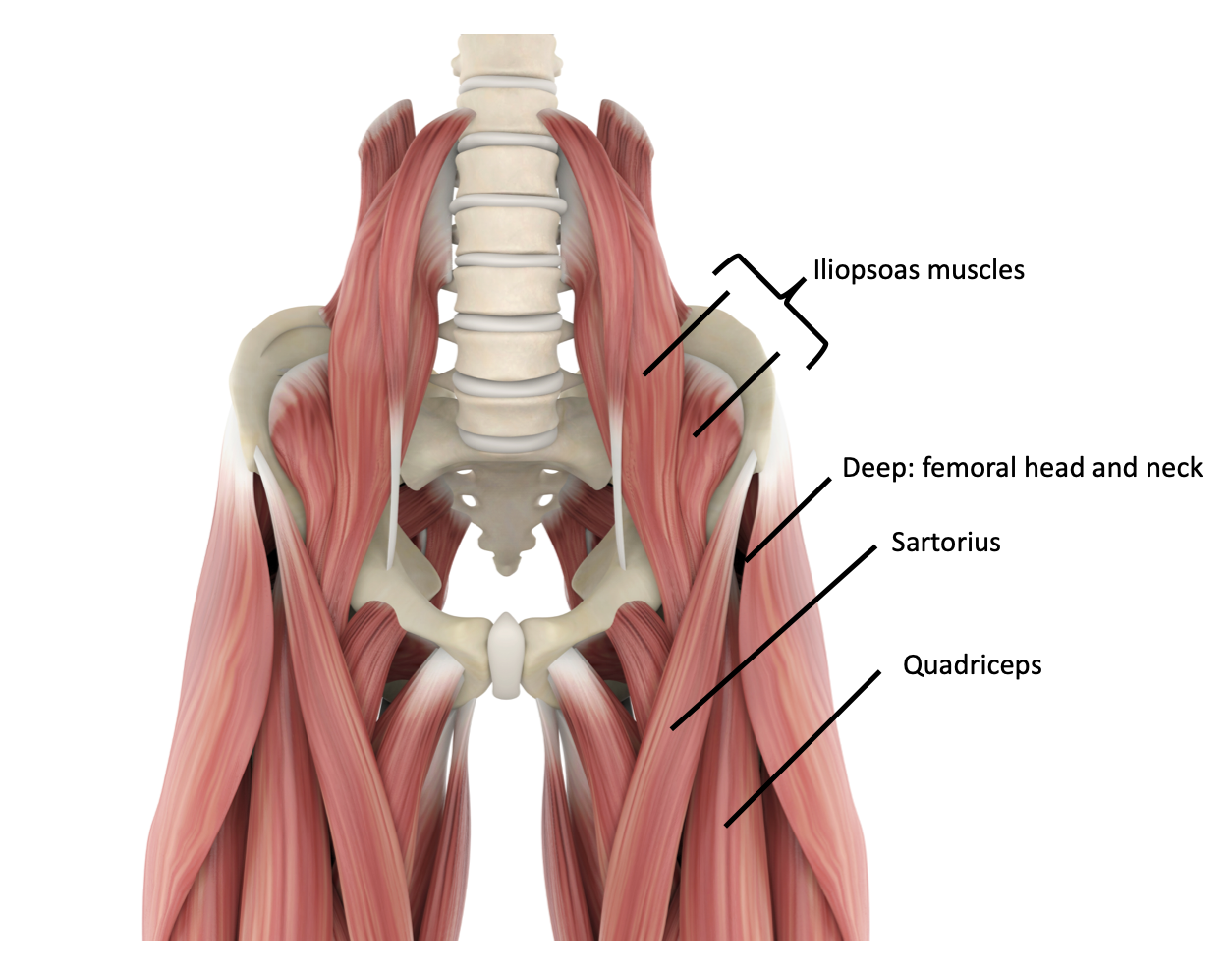
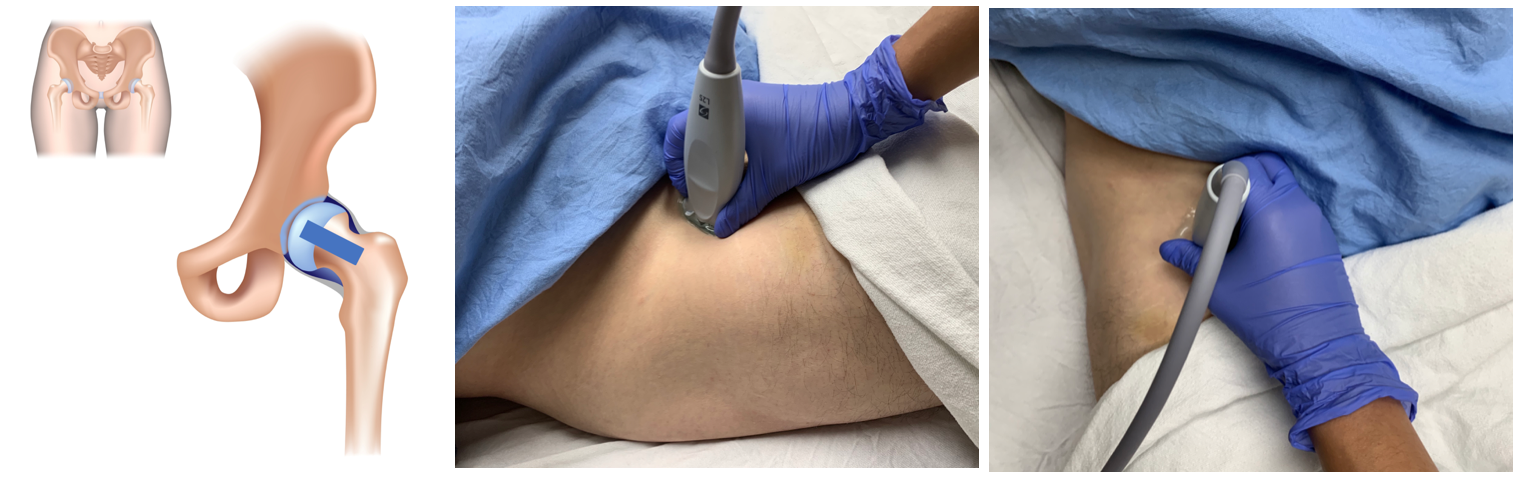
Figure 6: Probe position for hip ultrasound
What am I looking at?
Figure 7: Labelled normal hip ultrasound.
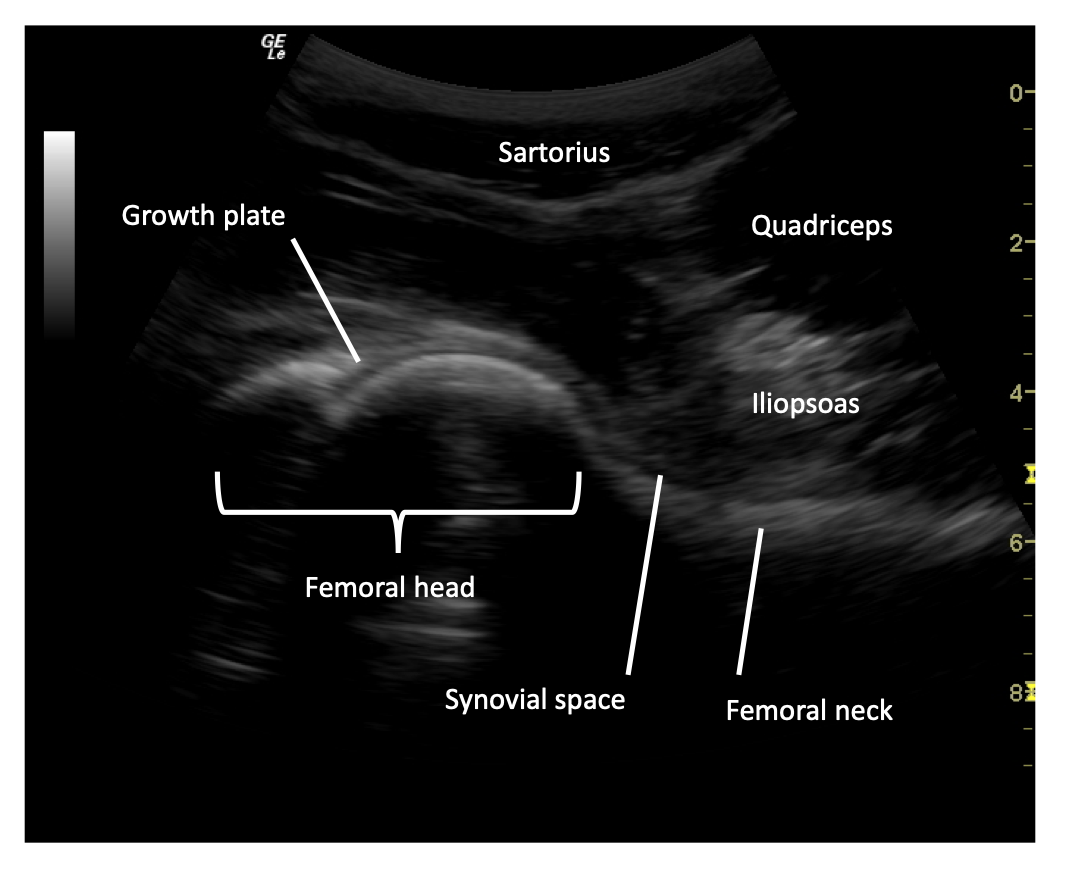
Femoral neck
Femoral head
Muscles
Synovial space
Normally, synovial fluid will follow the contours of the joint itself, in this case, the femoral head and neck. The size of a fluid collection in the hip is measured from the anterior surface of the femoral neck to the posterior surface of the iliopsoas muscle [4]. The space should be <5mm and within 2mm in comparison to the unaffected hip (Figure 8).
Figure 8: Normal hip ultrasound.

What is NOT normal?
The presence of a joint effusion in a hip is defined as a space between the anterior surface of the femoral neck to the posterior surface of the iliopsoas muscle of >5mm or >2mm difference in comparison to the unaffected side (Figure 9). An effusion will classically have a convex appearance (Video 1) in comparison to the normal concave appearance of the synovial fluid in a joint without an effusion.
Figure 9: Positive hip effusion.
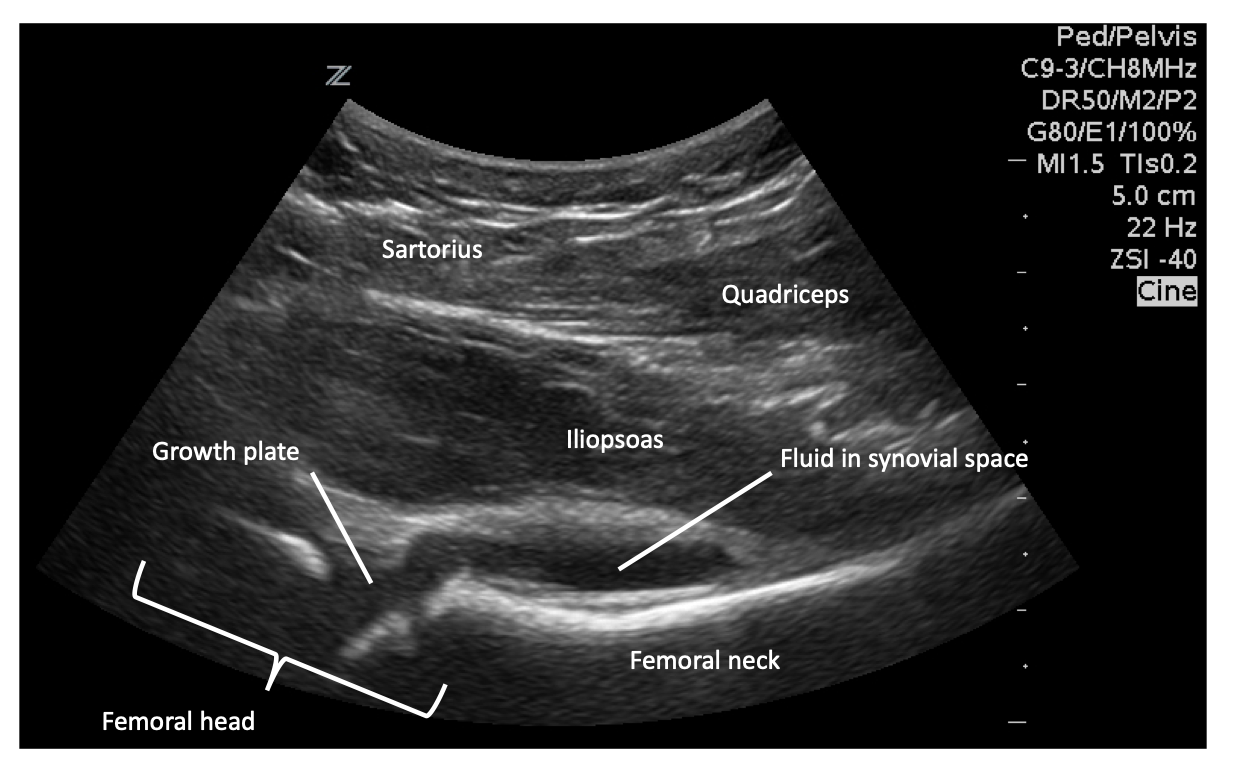
Video 1: Hip joint effusion. Note the convex appearance of the fluid on the image on the right.
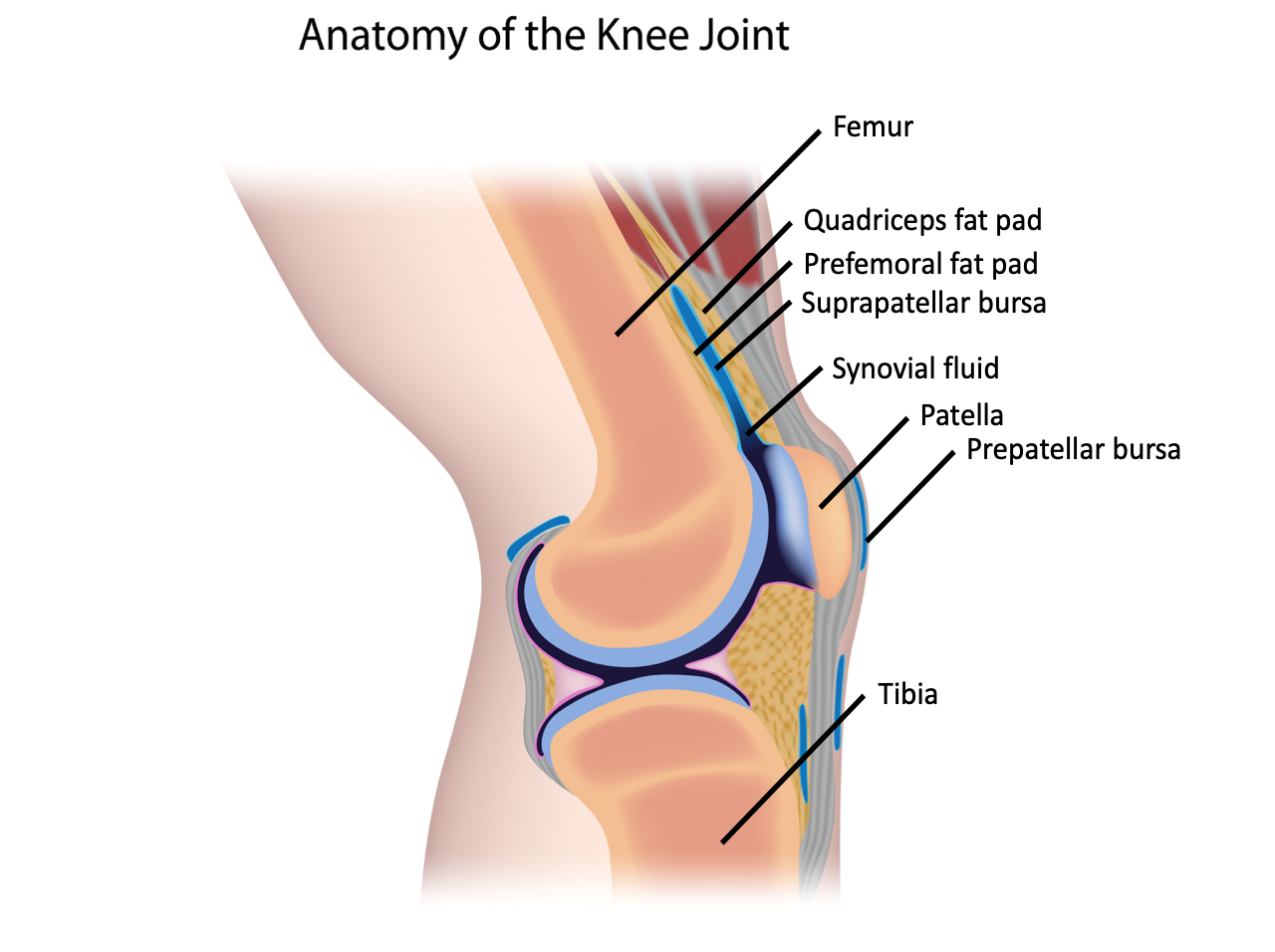
The knee is made up of the articulating surfaces of the femur and the tibia, with the patella lying anteriorly. The quadriceps tendon inserts on the patella, and the patellar tendon extends distally to the tibial tuberosity. The fluid within the synovial capsule is continuous with the suprapatellar bursa. The fat pads found within the knee joint include the quadriceps fat pad and the pre-femoral fat pad (Figure 10).
Figure 10: Anatomy of the knee joint.
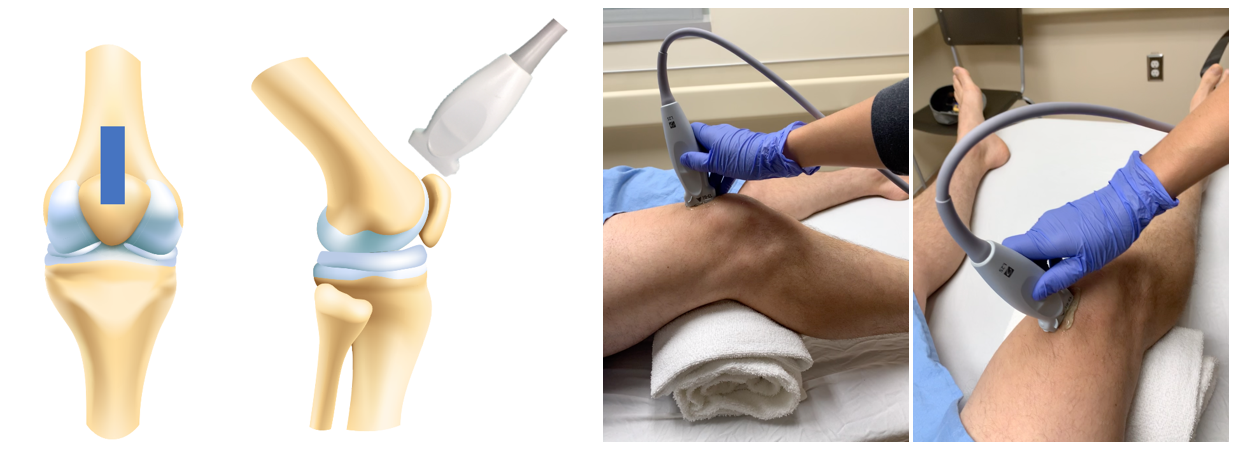
Technique
Figure 11: Probe position for knee ultrasound
What am I looking at?
Figure 12: Labelled normal knee ultrasound.
Patella
Femur
Quadriceps tendon
Fat Pads
Quadriceps fat pad – hyperechoic soft tissue collection just inferior to quadriceps tendon.
Suprapatellar bursa
Prepatellar bursa
Visualization of the knee joint in this view will show you the patella caudally and the femur extended cranially (Video 2). The quadriceps tendon will be a fibrous structure running in the near field (Figure 13). The suprapatellar bursa should be less than 2mm thick [1].
Video 2: Normal knee ultrasound.
Figure 13: Normal right and left knee ultrasound.
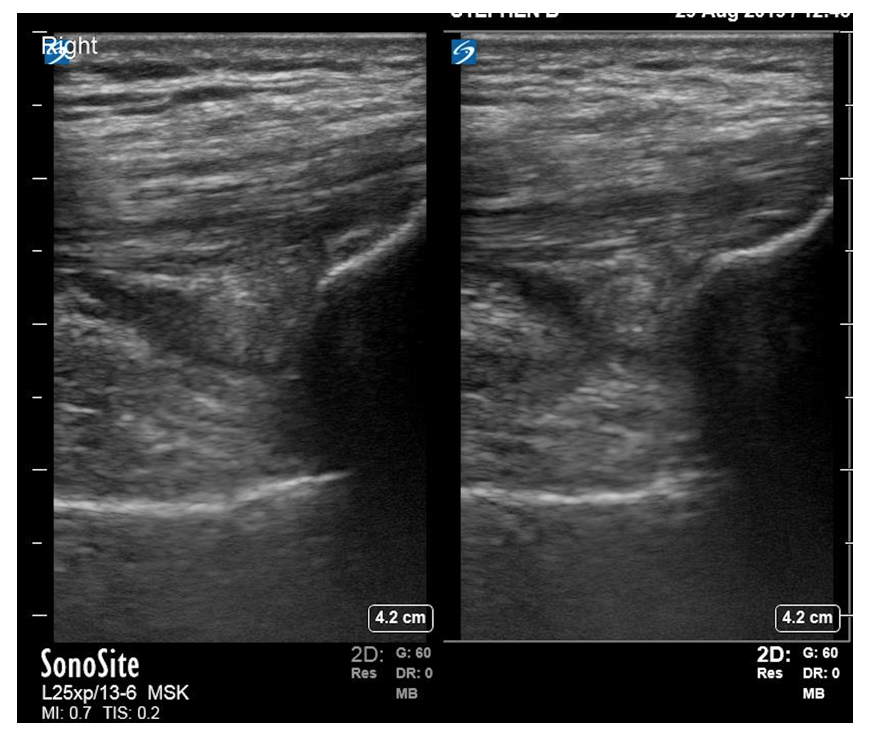
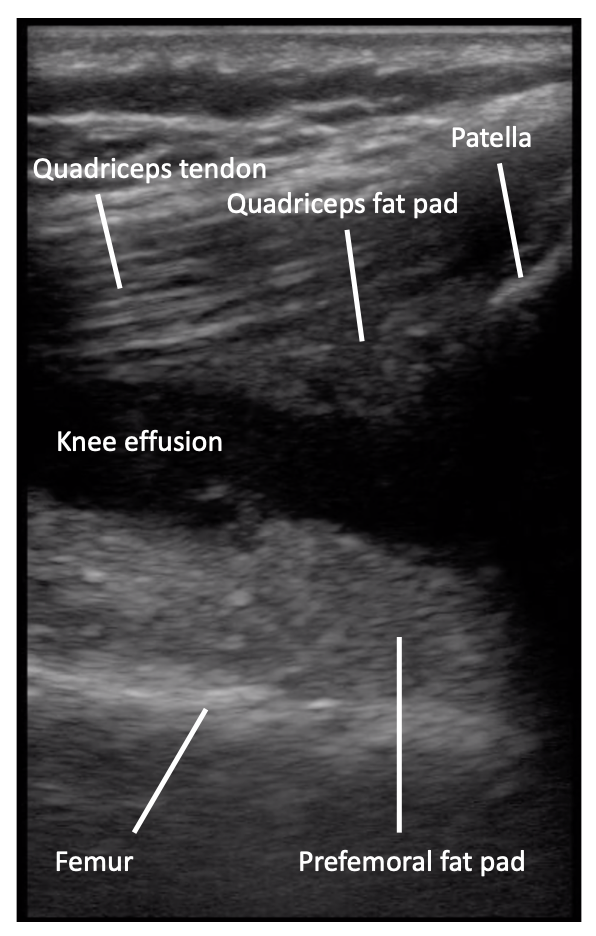
Fluid will collect in the suprapatellar bursa, found in between the prefemoral and quadriceps fat pads (Video 3). The ultrasound is positive for a knee effusion by a collection of hypoechoic fluid which is >2mm thick [1] (Figure 14). If you are not seeing any fluid collection, flexion of the knee can increase the fluid in the suprapatellar recess [13]. In addition, fluid can collect on both the medial and lateral side of the suprapatellar region, therefore scanning these areas can help identify fluid collections. To do this, slide the probe laterally and medially within the sagittal plane to identify hypoechoic fluid collections. This can help with performing ultrasound guided arthroscopy of the knee, although that is outside the scope of this module.
Video 3: Knee joint effusion. Note the fluid collection between the quadriceps fat pad and quadriceps tendon superiorly and the prefemoral fat pad inferiorly.
Figure 14: Positive knee effusion.
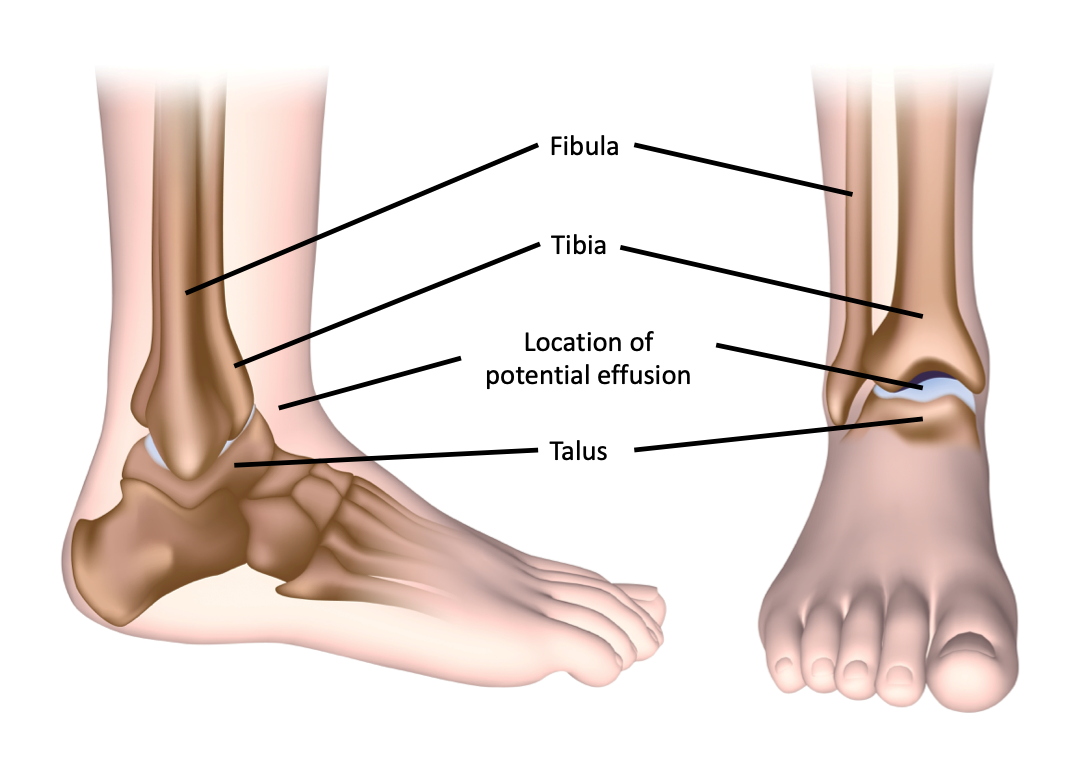
The area where an effusion in the ankle collects is at the intersection of the tibia and the talus (Figure 15). There is a fat pad (the anterior fat pad) at the junction of these two bones. Superficial to the boney surfaces, the tibialis anterior tendon is found.
Figure 15: Anatomy of the ankle joint.
Technique
Figure 16: Probe position for ankle ultrasound.

Figure 17: Labelled normal ankle ultrasound. Note that physiologic fluid and cartilage can appear similarly, so differentiate them with compression of the structures. Fluid will compress, cartilage will not.
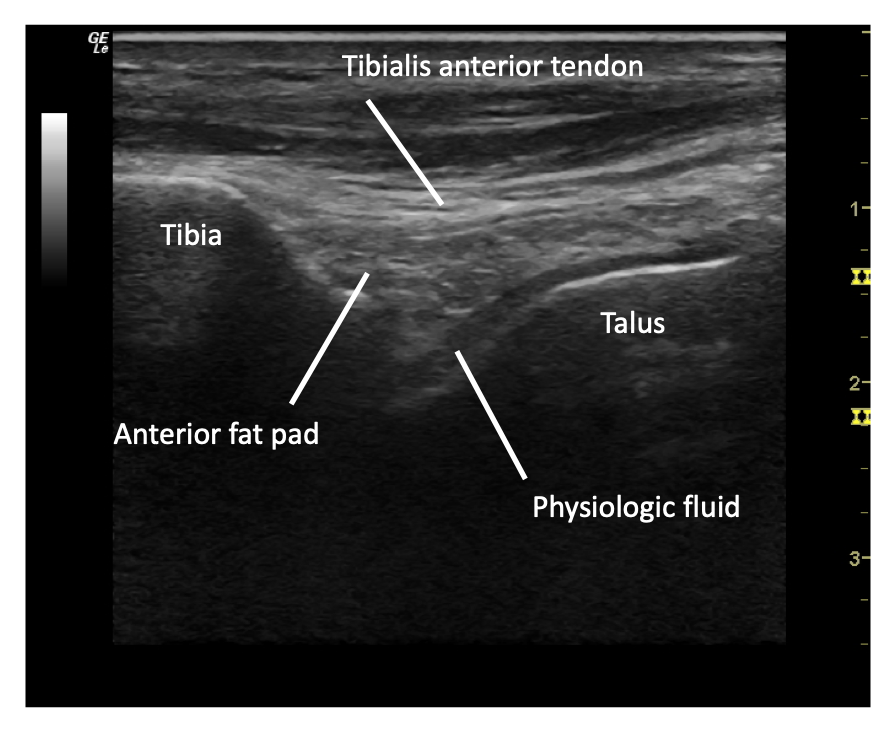
Tibia
Talus
Tibialis anterior tendon
Anterior fat pad
Anterior talotibial recess or synovial space
On ultrasound of the ankle, you will see the tibia extending cephalad and the joint line between the tibia and the talus (Video 4). Within the joint space, near field to the bony structures, there may be a small amount of physiologic fluid, and an anterior fat pad. As in the other joints, physiologic fluid will follow the contours of the bone, and have a more concave appearance (Figure 18).
Video 4: Normal ankle ultrasound.
Figure 18: Normal ankle ultrasound.
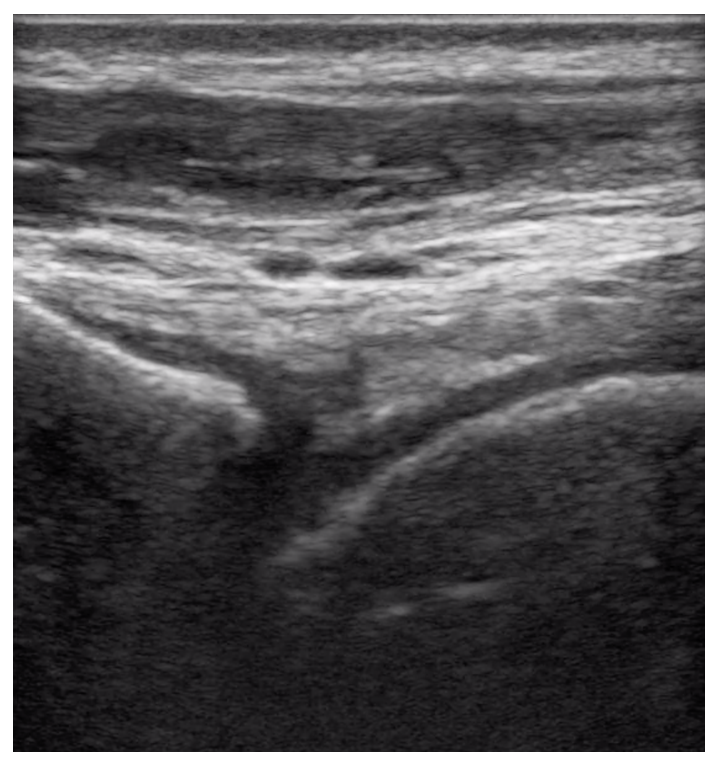
An ankle effusion is characterized by a convex shaped hypoechoic fluid collection anterior to the tibial and talar joint (Figure 19). In the ankle, unlike in the hip, there is no specific measurement for a positive effusion – the important feature to look for is the convexity of the collection (Video 5).
Figure 19: Positive ankle effusion.
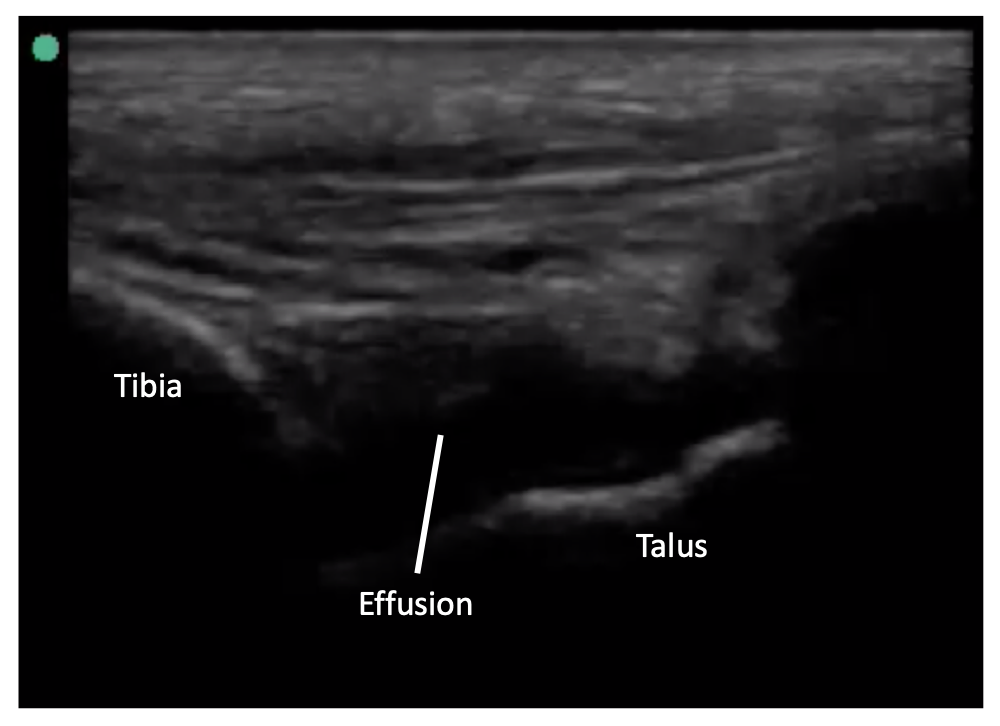
Video 5: Ankle joint effusion. Again, note the convex appearance of the fluid.
Ultrasound to identify joint effusions is widely used to assess those children presenting with a limp, refusal to weight bear or with a painful or swollen joint. PoCUS can be used to rapidly evaluate these children at the bedside thereby expediting management. This may include early referral to orthopedics. The use of PoCUS has also been shown to improve the ability of physicians performing arthrocentesis on joint effusions. PoCUS improves accuracy and decreases patient pain, without increasing the length of time required to perform the procedure [11,12].
Children often present to the emergency department with a limp, a painful joint, or refusal to weight bear. The differential is broad, including transient synovitis, septic arthritis and trauma. Previously, a formal ultrasound done by the radiology department has been used to determine the presence or absence of an effusion in order to help narrow the differential. PoCUS has been increasingly used by pediatric emergency physicians to quickly assess for the presence of a joint effusion at the bedside. The rapid identification of an effusion can expedite necessary interventions, including consultation of subspecialists or arranging for arthrocentesis.
Currently, most children presenting with a limp, refusal to weight bear or joint pain and swelling receive some combination of x-ray, blood work and formal ultrasound in the radiology department. Ultrasound as an imaging modality has many advantages, including low cost and no radiation [1,2]. The use of ultrasound at the bedside provides many advantages in its ease of access, as well as speed and portability [1-2]. This is especially useful when children are presenting to the department outside the hours in which a formal ultrasound is readily available.
Physical examination for joint effusions can be limited by pain, patient cooperation or soft tissue changes. POCUS is superior to physical exam for the detection of effusions and can be used to differentiate swelling at a joint due to effusion and soft tissue change (e.g. cellulitis) [3]. From an imaging perspective, X-ray has been shown to have a sensitivity for identifying an effusion ranging between 20-28%, whereas the sensitivity of a formal ultrasound approaches 100% [4-5]. Many studies have shown that PoCUS can been used by emergency physicians to easily identify fluid or a joint effusion in the hip, knee and ankle [1,5,6,7]. For example, a study in 2010 comparing trained PEM physicians performing hip ultrasound to a formal ultrasound read by radiologists showed a sensitivity of 80% and specificity of 98%. Moreover, when the physician reported confidence in their exam, the specificity and positive predictive value improved to 100% [7]. In 2018 Cruz et al showed that PEM physicians were able to detect hip joint effusions with a sensitivity of 85% and specificity of 98% [2]. In 2010 Adhikari and Blavais examined the role of PoCUS in patients presenting with joint complaints. In patients with clinically suspected effusions in whom arthrocentesis was planned, management changed in 69.2% after PoCUS was performed. In those in whom arthrocentesis was not planned, management changed in 53.3% of cases after PoCUS was performed [8]. Clinically, the absence of a joint effusion can effectively rule out septic arthritis, which can prevent unnecessary interventions on patients.
Overall, the use of POCUS to identify joint effusions is safe, easy to perform, and a quick way to begin the work up for the child presenting to the emergency department with a limp.
Cellulitis can have a highly variable appearance. In general, the subcutaneous tissue appears thickened and will have a “cobblestone” appearance. This is caused by subcutaneous edema and inflammation generated by the surrounding infection. Cobblestoning is not a specific finding to cellulitis but a finding in tissue edema, care must be taken to correlate to the clinical scenario. If uncertain, compare the area of interest to an unaffected area of skin.
Figure 3: Cobblestoning
| Cobblestone appearance of cellulitis | Cobblestone sidewalk |
 |
 |
Video 4: Soft tissue cobblestoning
Edema from any source including:
Abscesses appear as heterogeneous anechoic, isoechoic (gray) or hypoechoic fluid collections. Their appearance is often not uniform. Abscesses can be well-circumscribed or be irregularly shaped areas of fluid which may demonstrate posterior acoustic enhancement (bright white in the far field). As with cellulitis, measure the size of the abscess in both the transverse and longitudinal plane. There is some evidence from an immunocompetent pediatric emergency department population that abscesses larger than 5 cm in diameter predict need for hospitalization [14]. In addition, measure the depth from the skin and the width from the base in order to guide future attempts at incision and drainage. As part of the evaluation, apply firm and graded pressure with the probe over the abscess to look for fluctuance (often over a point of maximal tenderness) and the “swirl sign.” Swirl sign refers to the movement of fluid and debris within the abscess and is generated by compression over the area. Finally, always evaluate the abscess with color Doppler to look for internal blood flow and surrounding vasculature prior to making an incision.
Video set 5: Examples of soft tissue abscesses
Courtesy of EDSONOshare library
Video 6: Video illustrating a positive “Swirl Sign”
| Practice Pearl: Prior to performing any incision and drainage of an abscess, use color Doppler to look for evidence of blood flow. In addition, color Doppler can be used to identify surrounding blood vessels in order to decrease the rate of procedural complications. |
Figure 4: Color Doppler over a suspected abscess

This mass was a clinically suspected abscess but bedside PoCUS identified significant blood flow. Planned incision was aborted and the patient was referred to surgery for further management.
Due to the low incidence and high morbidity of necrotizing soft-tissue infections, it remains a diagnosis that requires physicians to maintain a high clinical index of suspicion. The use of bedside ultrasound should never delay surgical consultation for these patients but should instead be used to expedite diagnosis. There are three main sonographic findings in necrotizing fasciitis. These include subcutaneous air (often tracking along a fascial plane) with accompanying “comet-tail” artifact, diffuse subcutaneous tissue thickening (which often requires comparison to a contralateral side), and >5mm of fluid accumulation along a facial plane [10].
Figure 5: Sonographic findings suggestive of necrotizing infection
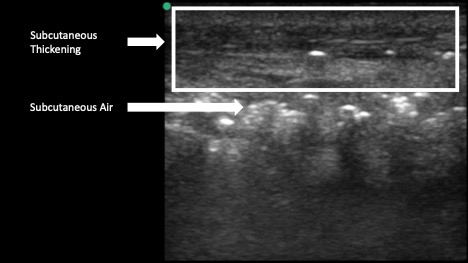

Video 7: PoCUS suggesting necrotizing infection
Courtesy of EDSONOshare Library
Research has shown that over one-third of hand foreign bodies are missed at the index visit. Bedside ultrasound can be used to both diagnose foreign bodies and plan removal by accurately identifying the depth of the target and surrounding structures which may need to be avoided (i.e., vasculature). Ultrasound is superior to plain films for radiolucent objects such as plastic, wood or plant matter. When using ultrasound to guide removal of a foreign body, be sure to measure the distance from the skin surface with the calipers and scan the object in 2 planes to fully characterize its length, depth and width.
| Practice Pearl: When using ultrasound to guide removal of a foreign body, consider placing multiple high gauge needles to mark the location of the object prior to dissecting down to find and then remove the foreign body. This can save a lot of time and avoid unnecessarily damaging tissue. |
Figure 6: Foreign bodies on bedside ultrasound
| Wood | Glass | Metal |
 |
 |
 |
| Wood often demonstrates attenuation artifact or acoustic shadow. | Glass often demonstrates reverberation or comet tail artifact. | Metal often demonstrates reverberation artifact on ultrasound. |
Video set 8: Soft tissue foreign bodies
Wood
Glass
Metal
Courtesy of EDSONOshare library