What Am I Looking At?
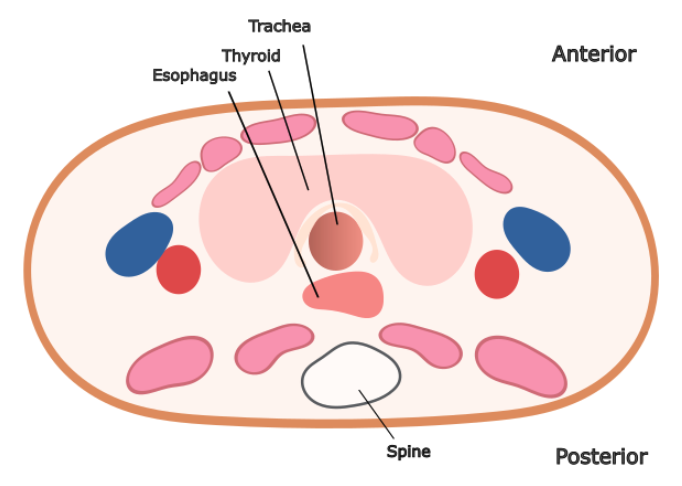
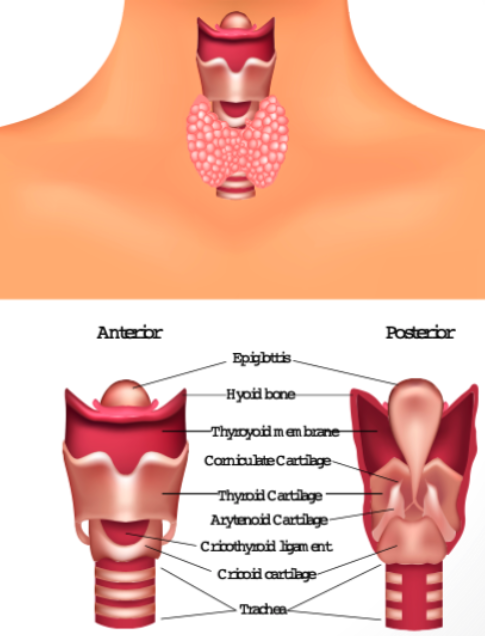
Key anatomical structures relevant to airway management include the trachea, esophagus, thyroid gland, thyroid cartilage, vocal cords, cricothyroid membrane, and cricoid cartilage.
In cross-section, the trachea is midline, and the esophagus lies posterolateral, usually to the left. The thyroid gland sits anteriorly, partially wrapping around the trachea (Figure 1)
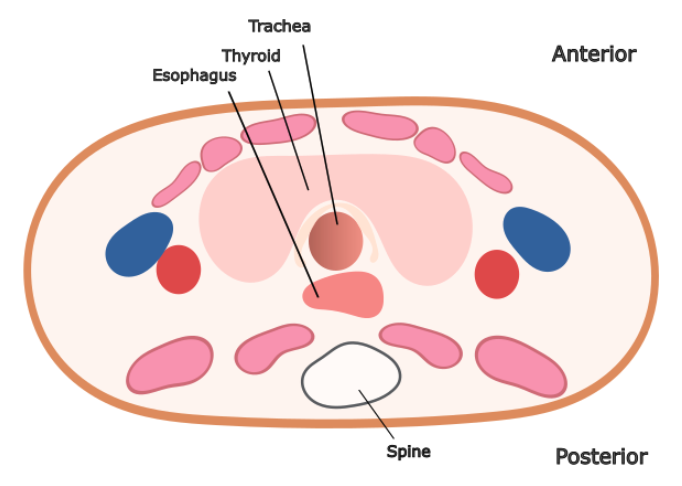
Figure 1: Cross sectional anatomy on the neck in axial plane
Additional anatomical landmarks relevant for surgical airway planning, from cephalad to caudad, include the thyroid cartilage, cricothyroid membrane, cricoid cartilage and trachea (Figure 2)
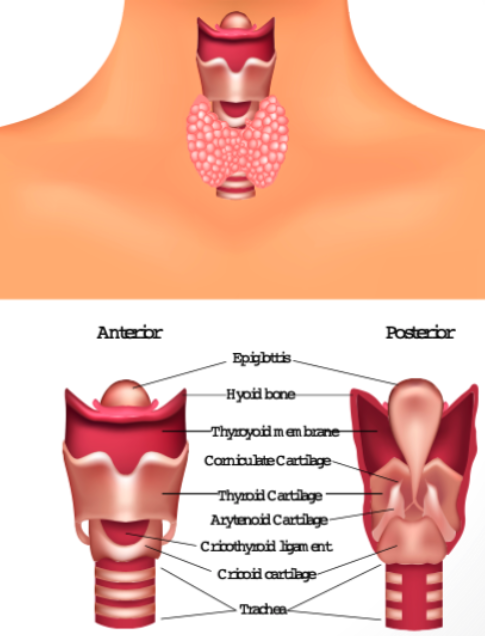
Figure 2: Longitudinal Anatomy relating to surgical airway planning.
Ultrasound Anatomy Review
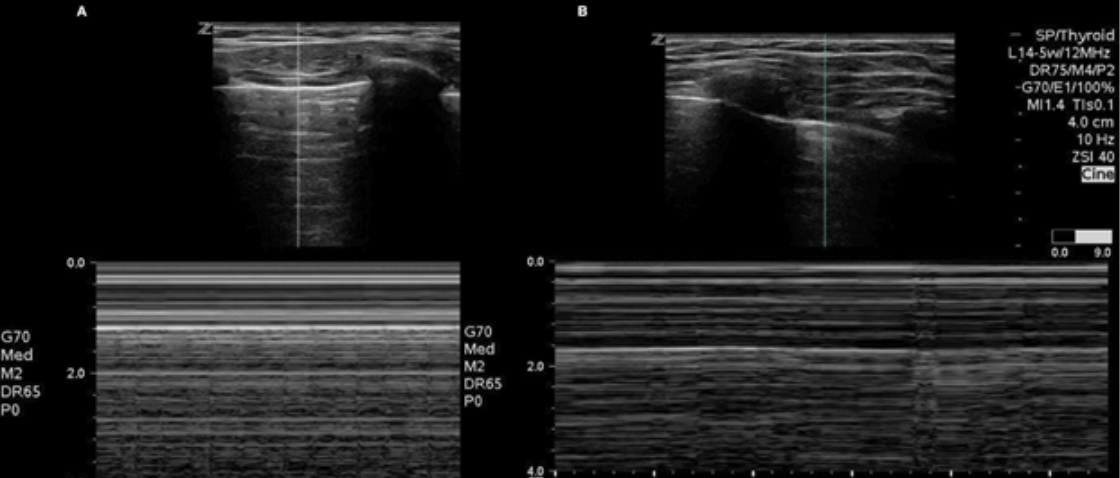
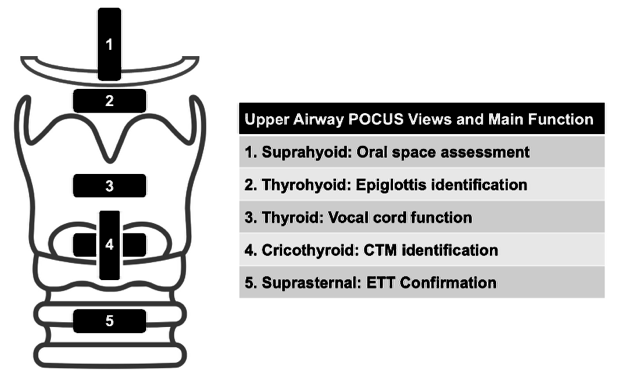
The airway can be evaluated by ultrasound from the suprahyoid area to the suprasternal notch in both the transverse and longitudinal planes (figure 3).
The transverse view is most used to confirm the location of the ETT (Figure 4), but the longitudinal view can aid in landmarking when planning a surgical airway (Figure 5).
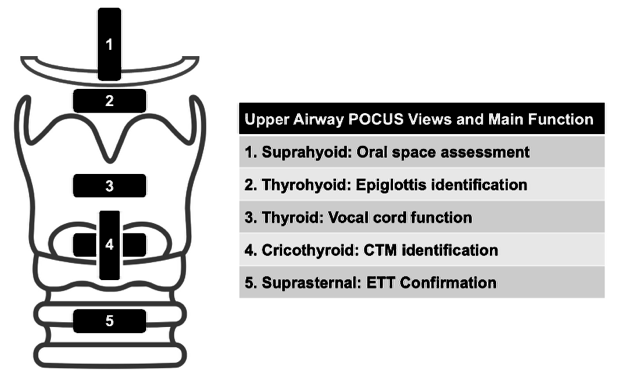
Figure 3. Reproduced from Lin et al, Diagnostic 2023 [19]
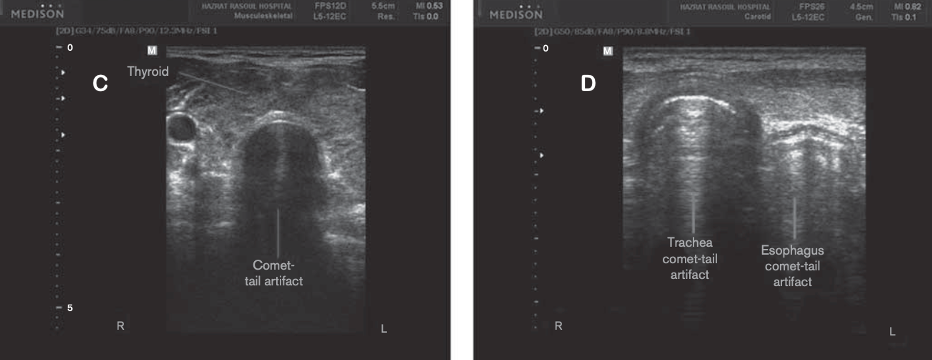
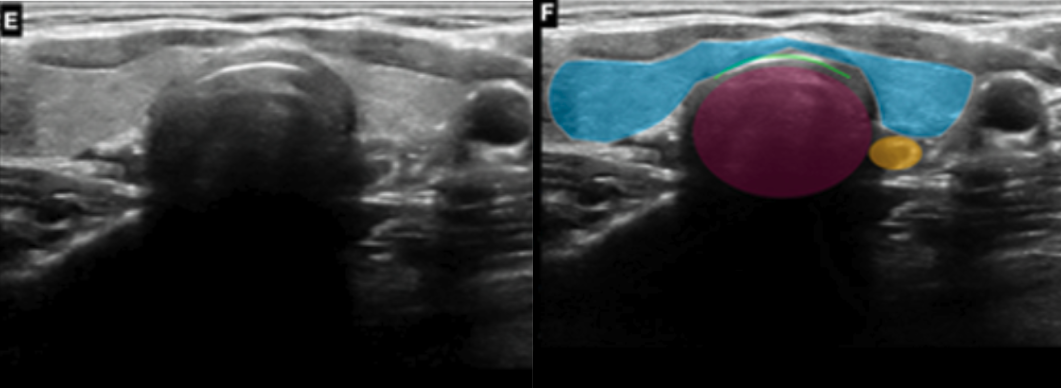
Transverse view:
In this view, we see the trachea centrally, and the esophagus lies posterolateral (left). The thyroid gland sits anteriorly wrapping around the trachea.
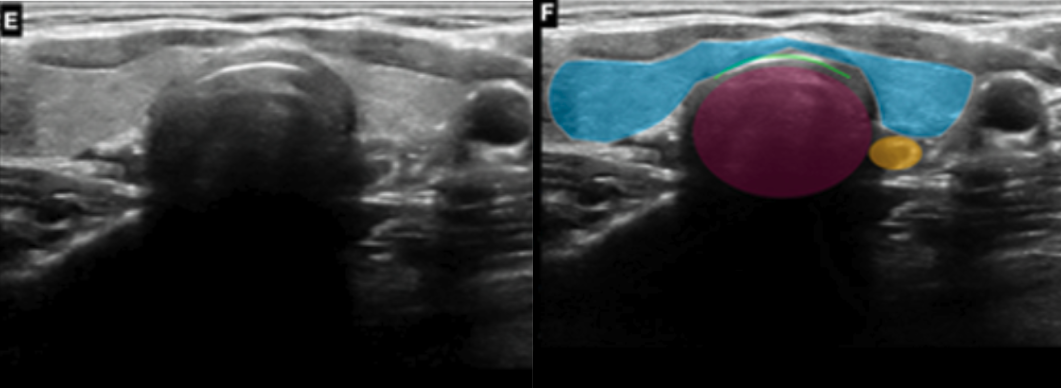
Figure 4: Transverse plane over the suprasternal notch showing the trachea (purple circle), esophagus (yellow circle) and thyroid (blue area) with the air-mucosa interface (green line).
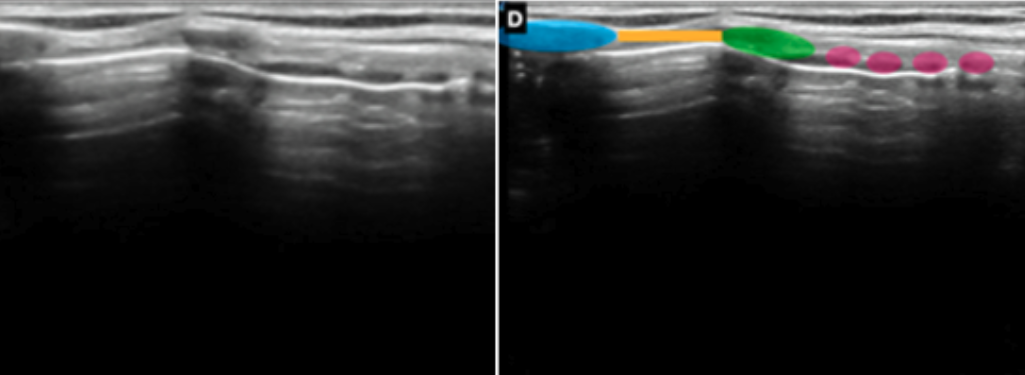
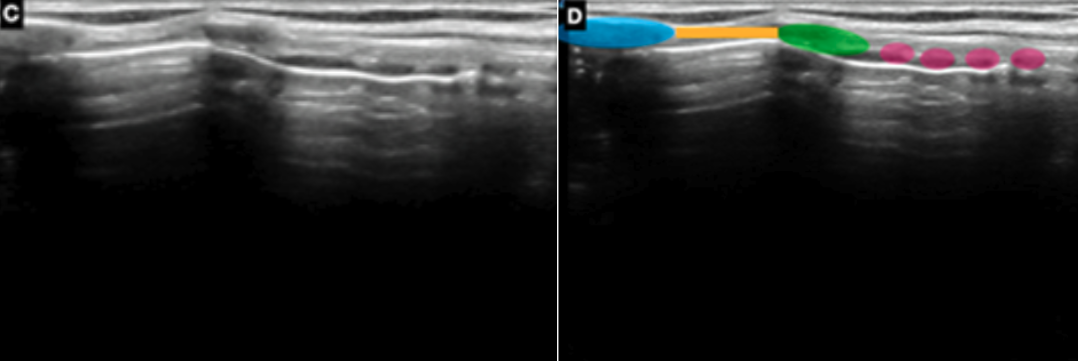
Longitudinal View
In this view, the thyroid cartilage, cricothyroid membrane, cricoid cartilage and tracheal rings (string of pearls) are seen.
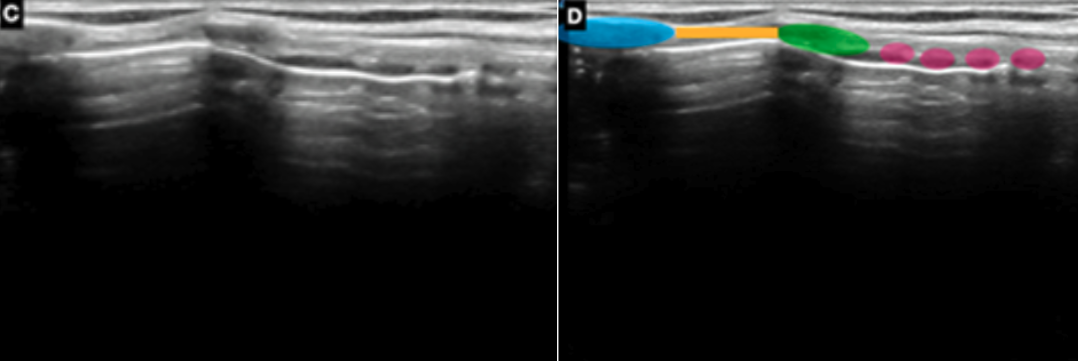
Figure 5: Longitudinal plane over the cricothyroid membrane (yellow line), thyroid cartilage (blue circle), cricoid cartilage (green circle) and tracheal rings string of pearls (purple circles).