**To unlock access to the first quiz, make sure to select the “Mark as Completed” button below
References
- Sullivan R, Baston CM. When Not to Trust the Bladder Scanner. The Use of Point-of-Care Ultrasound to Estimate Urinary Bladder Volume. Ann Am Thorac Soc. 2019 Dec;16(12):1582–4.
- Taus PJ, Manivannan S, Dancel R. Bedside Assessment of the Kidneys and Bladder Using Point of Care Ultrasound. POCUS J. 2022 Feb 1;7(Kidney):94–104.
- Dessie A, Steele D, Liu AR, Amanullah S, Constantine E. Point-of-Care Ultrasound Assessment of Bladder Fullness for Female Patients Awaiting Radiology-Performed Transabdominal Pelvic Ultrasound in a Pediatric Emergency Department: A Randomized Controlled Trial. Annals of Emergency Medicine. 2018;72(5):571-580. doi:1016/j.annemergmed.2018.04.010
- O’Brian RA, Firan A, Sheridan MJ, Kou M, Place RC, Chung CH. Bladder Point-of-Care Ultrasound: A Time Saver in the Pediatric Emergency Department. The Journal of Emergency Medicine. 2021;61(3):e32-e39. doi:1016/j.jemermed.2021.04.010
- Ho-Gotshall S, Wilson C, Jacks E, Kashyap R. Handheld Ultrasound Bladder Volume Assessment Compared to Standard Technique. Cureus [Internet]. 2024 Jul 16 [cited 2025 Apr 10]; Available from: https://www.cureus.com/articles/180394-handheld-ultrasound-bladder-volume-assessment-compared-to-standard-technique
- Medical Advisory Secretariat. Portable bladder ultrasound: an evidence-based analysis. OntarioHealth TechnologyAssessmentSeries 2006; 6(11)
- Akca Caglar A, Tekeli A, Karacan CD, Tuygun N. Point-of-Care Ultrasound-Guided Versus Conventional Bladder Catheterization for Urine Sampling in Children Aged 0 to 24 Months. Pediatr Emerg Care. 2021 Aug;37(8):413–6.
- Chen L, Hsiao AL, Moore CL, Dziura JD, Santucci KA. Utility of Bedside Bladder Ultrasound Before Urethral Catheterization in Young Children. Pediatrics. 2005 Jan 1;115(1):108–11.
- Marzuillo P, Guarino S, Capalbo D, et al. Interrater reliability of bladder ultrasound measurements in children. Journal of Pediatric Urology. 2020;16(2):219.e1-219.e7. doi:10.1016/j.jpurol.2019.12.015
- Ma J, Mateer J. Ma and Mateer’s Emergency Ultrasound. 4e ed. USA: McGraw Hill; 2021
- Jade Deschamps, Vi Dinh. Bladder Ultrasound Made Easy: Step-By-Step Guide [Internet]. POCUS 101. Available from: https://www.pocus101.com/bladder-ultrasound-made-easy-step-by-step-guide/
- Lim LY, Chang SJ, Yang SSD. Age- and gender-specific normal post void residual urine volume in healthy adolescents. J Pediatr Urol. 2023 Aug;19(4):367.e1-367.e6.
- Chang S, Chiang I, Hsieh C, Lin C, Yang SS. Age‐ and gender‐specific nomograms for single and dual post‐void residual urine in healthy children. Neurourol Urodyn. 2013 Sep;32(7):1014–8.
- Chang SJ, Yang SSD. Variability, Related Factors and Normal Reference Value of Post-Void Residual Urine in Healthy Kindergarteners. J Urol. 2009;182(4S):1933-1938. doi:10.1016/j.juro.2009.02.086


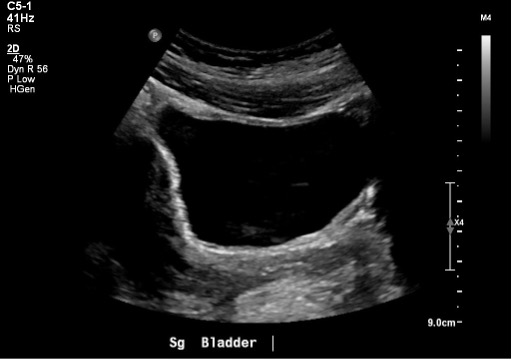 Figure 10: Normal bladder in the sagittal plane
Figure 10: Normal bladder in the sagittal plane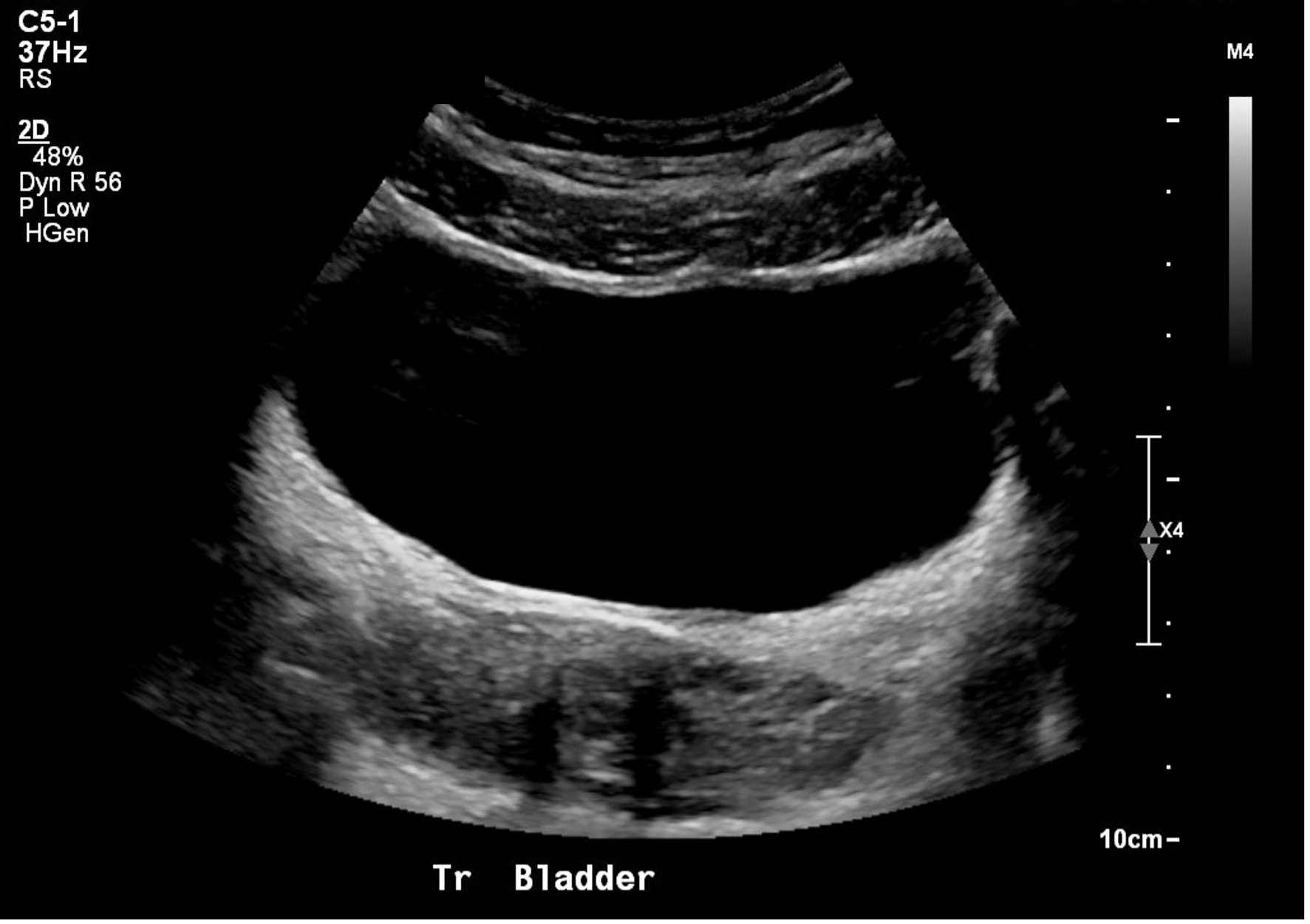
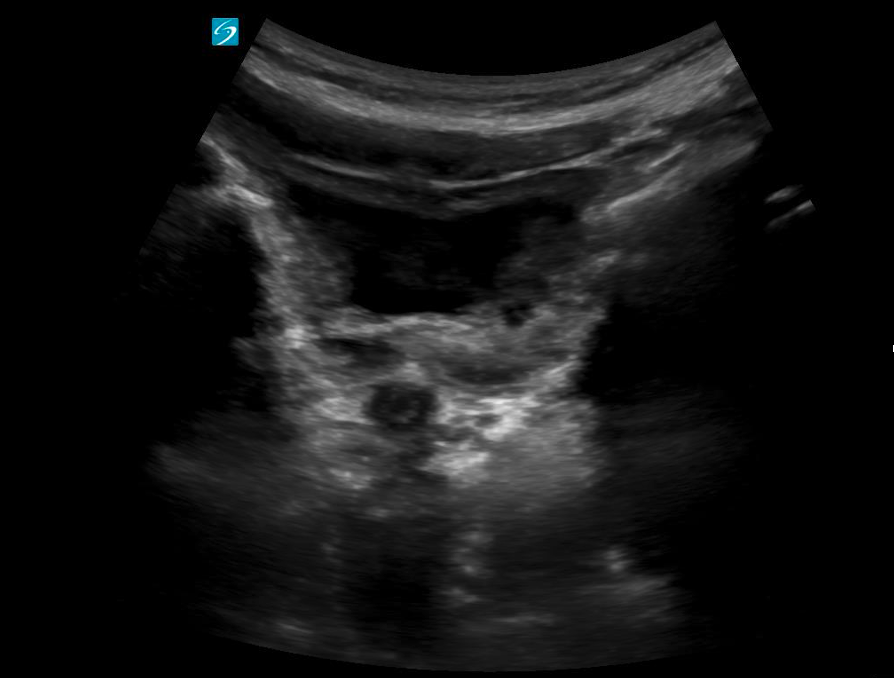 Figure 12: Transverse view of a near empty bladder with thicker walls
Figure 12: Transverse view of a near empty bladder with thicker walls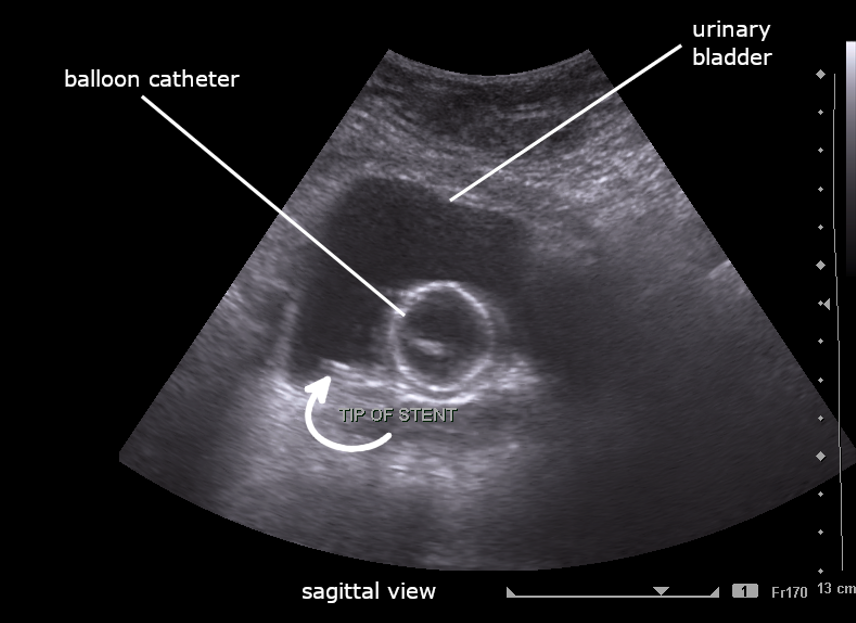
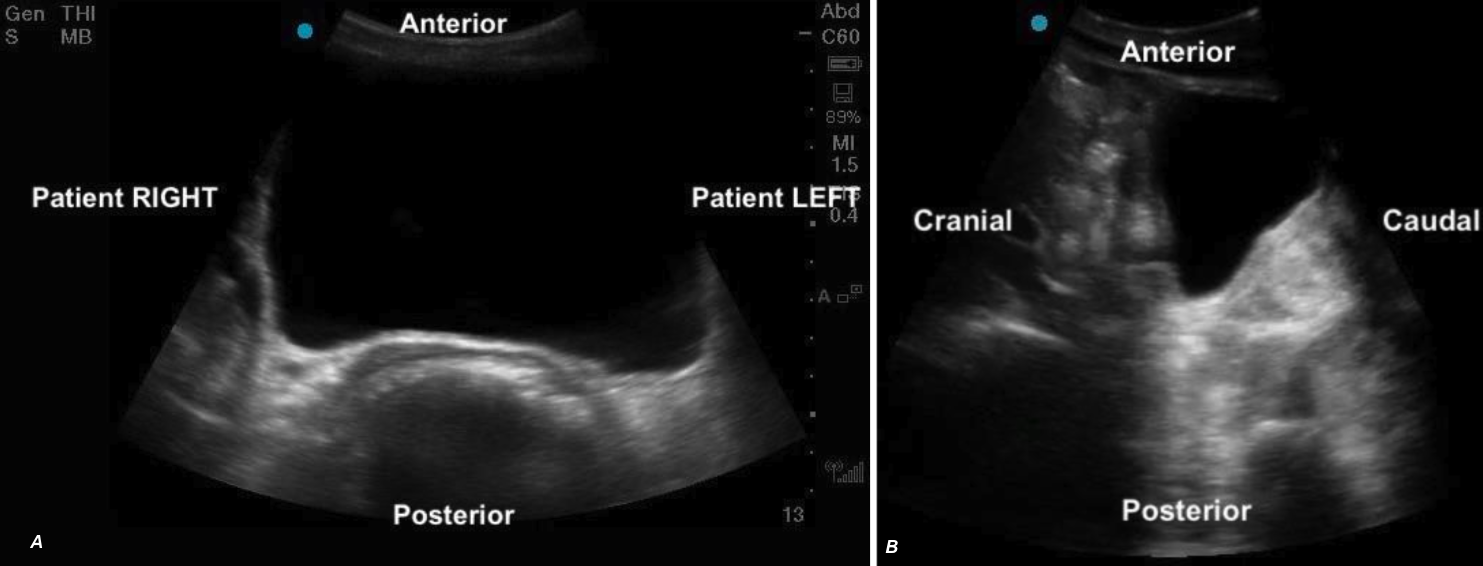 Figure 5ab: Transverse and sagittal bladder views with orientation labels
Figure 5ab: Transverse and sagittal bladder views with orientation labels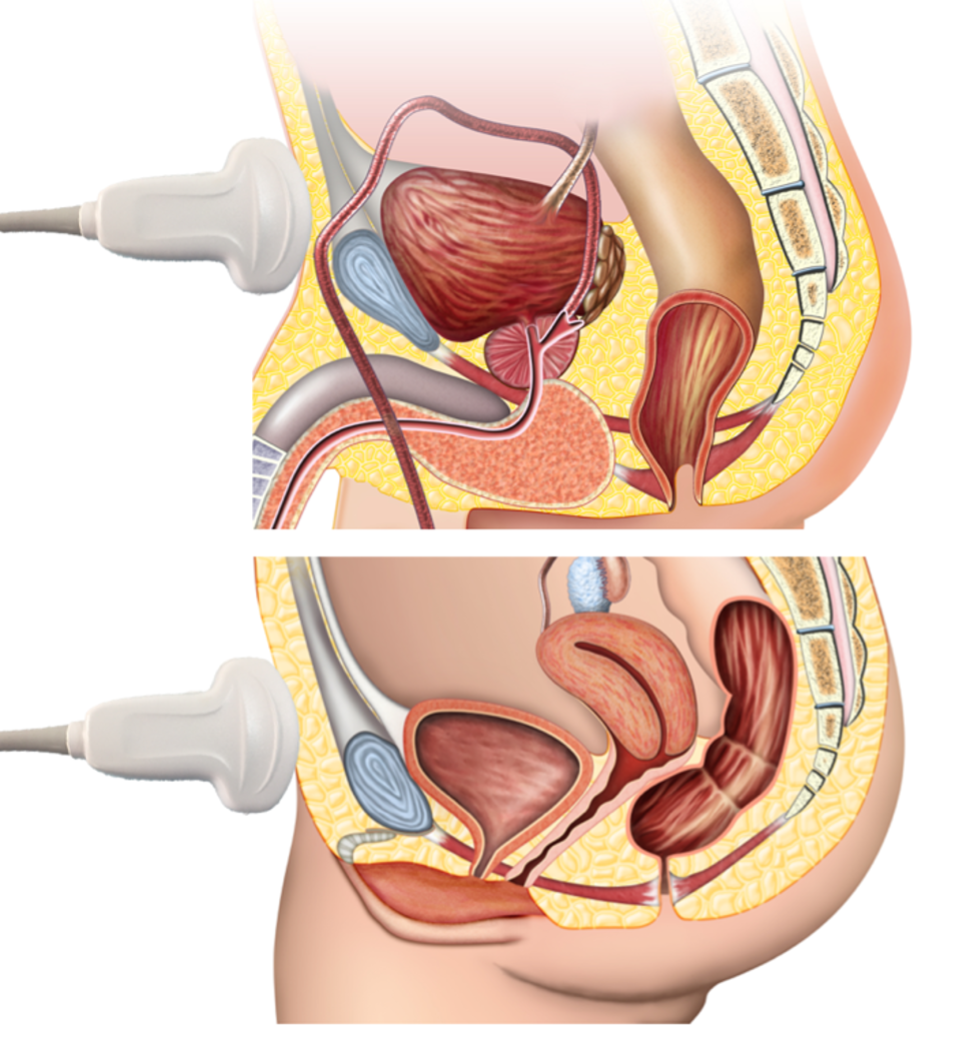
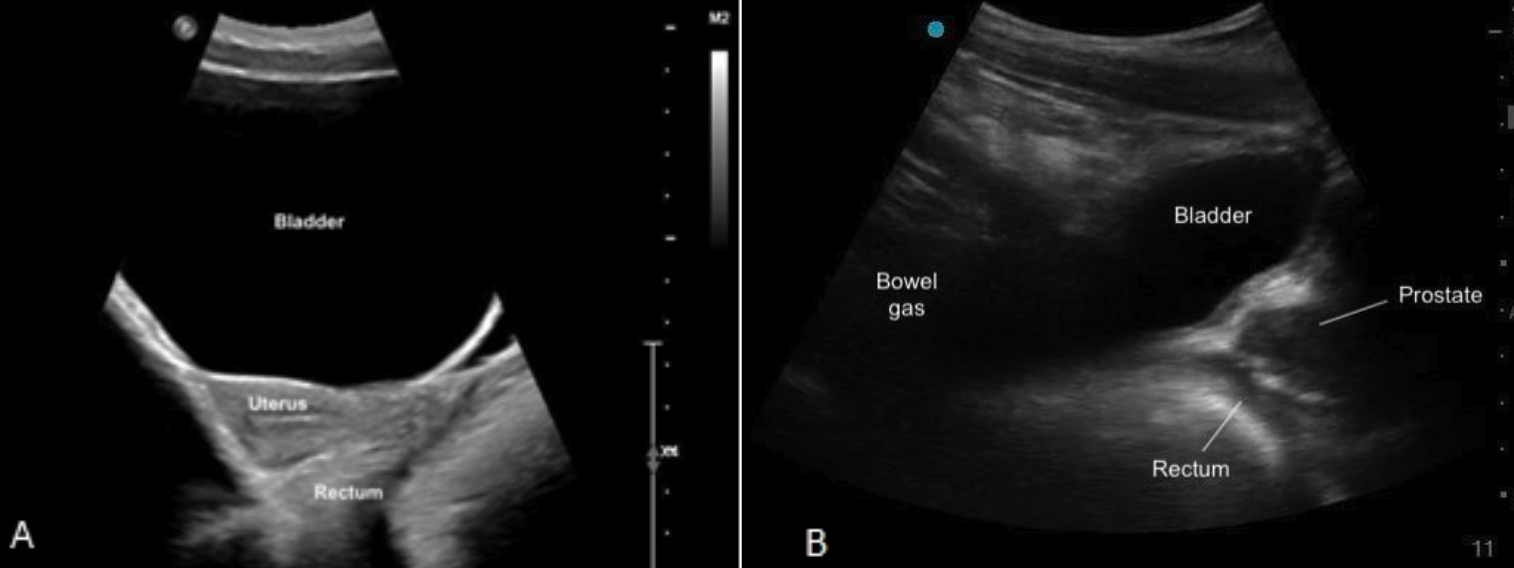

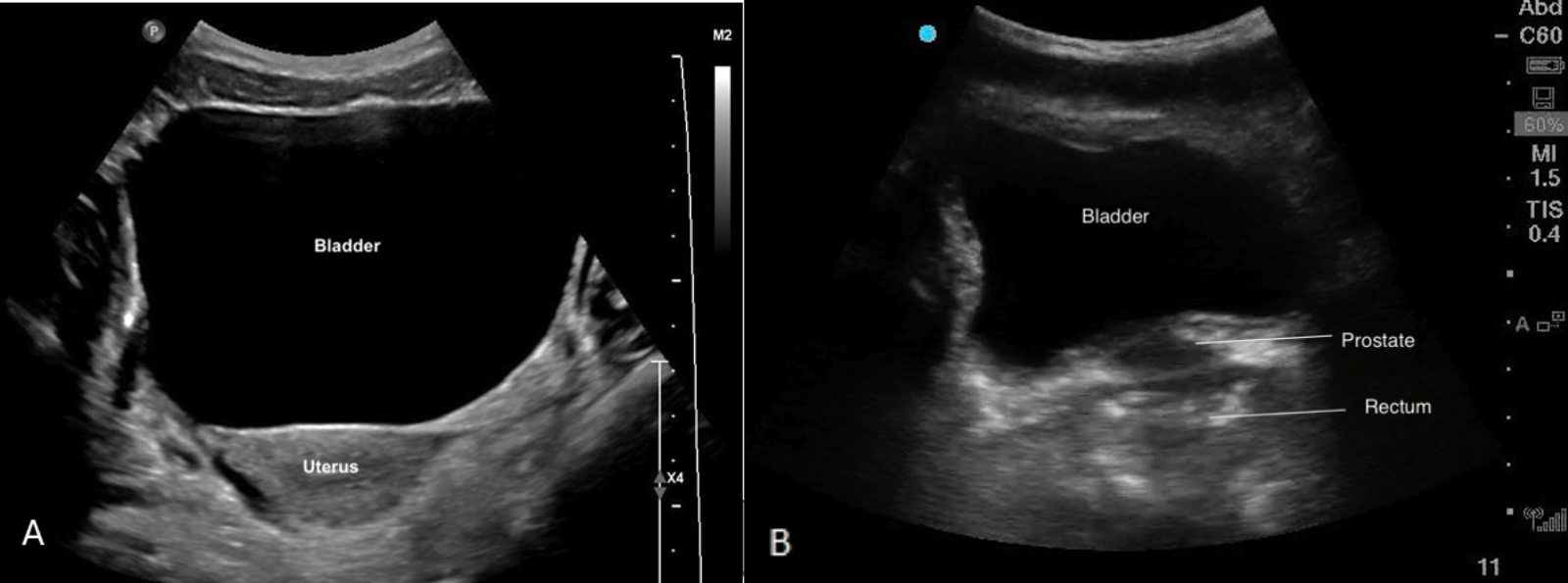
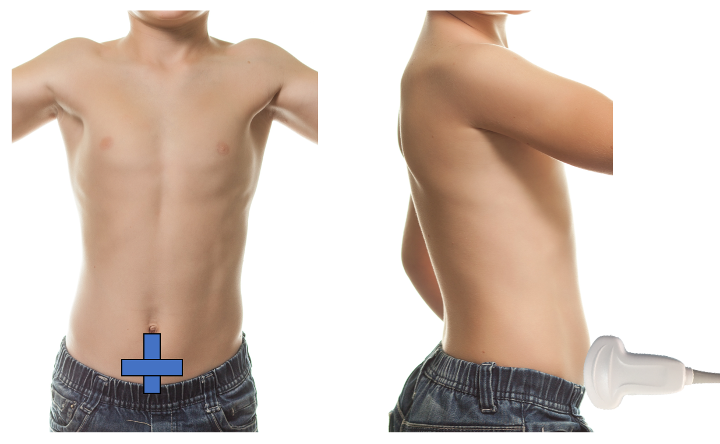
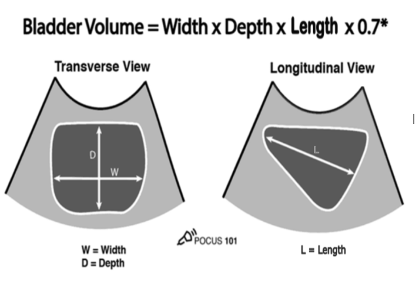
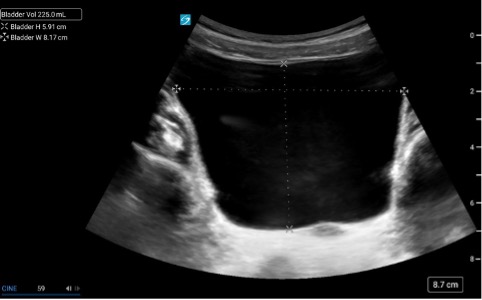 Figure 3.
Figure 3. 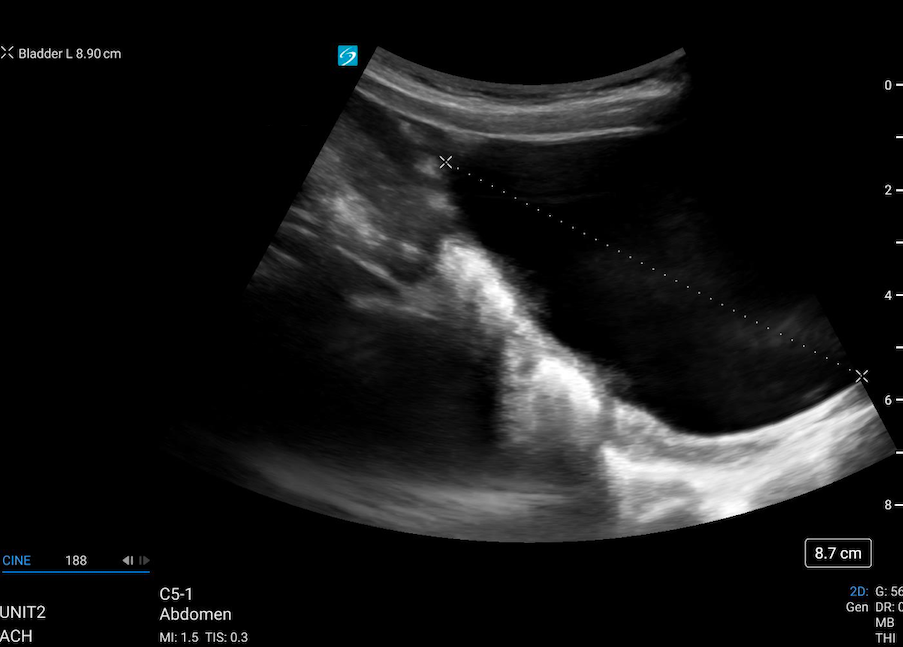 Figure 4.
Figure 4. 