What is normal?
In normal lung, the pleura is easily visualized as ultrasound waves are deflected by aerated lung. Reverberation artifacts from the pleural line (secondary to the significant change in acoustic impedance at the pleural-lung interface) generate horizontally arranged artifacts called A-lines (figure 2). Other normal structures visualized are the rib and corresponding rib shadowing below, and at the base of the lung the double line of the diaphragm muscle (figure 3).
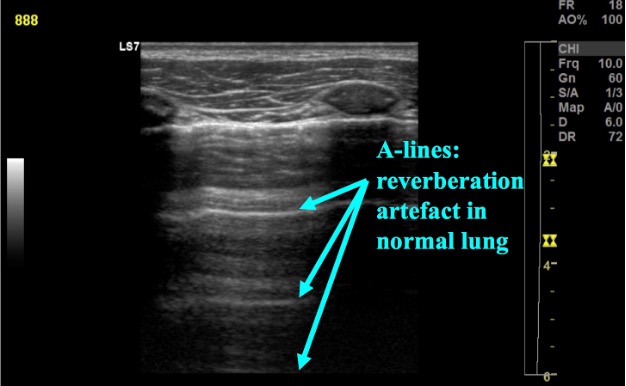
Figure 2: Normal lung with a-line reverberation artefact
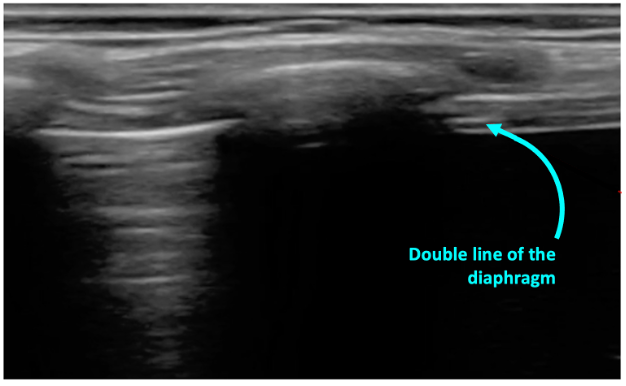
Figure 3: Normal lung base with the beginning of the diaphgram noted on screen right
