2D Findings: Testicular orientation, volume and texture
Orientation: In testicular torsion, the affected testicle often lies horizontally
Volume: In acute torsion, the testicle is enlarged with increased volume (Video 2). In chronic or missed torsion the testicle undergoes atrophy, leading to a decrease in volume. Unilateral increased volume of the testicle should raise suspicion for partial torsion or torsion-detorsion in the right clinical context but may also be seen in orchitis.
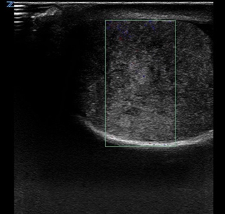
Texture: Testicular heterogeneity (figure 6) is typically a later finding and associated with worse outcomes, including non-viable testis (14). Testicular fragmentation and patching can be seen once the testicle becomes necrotic and increases the risk of testicular loss (figure 7)(15).
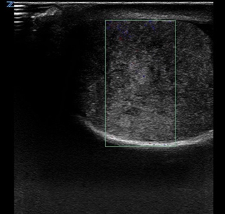
Figure 6. Heterogenous echogenicity of enlarged testicle
Figure 7. Testicular fragmentation (a,b) and patching (c,d)
Color Doppler
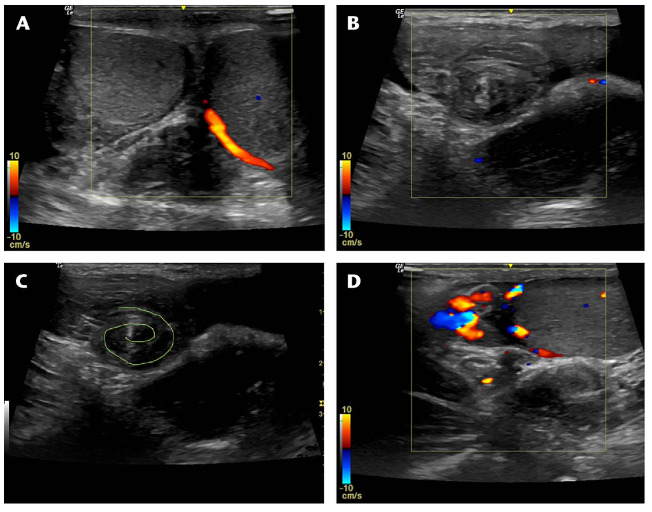
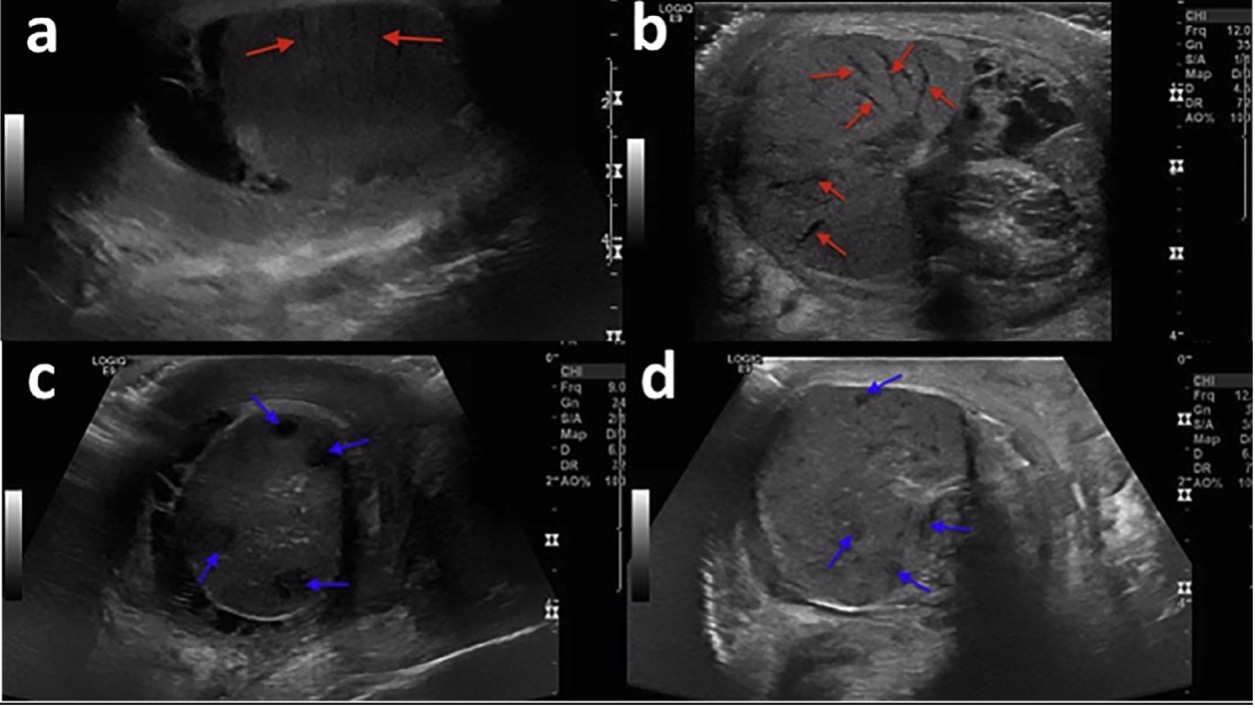
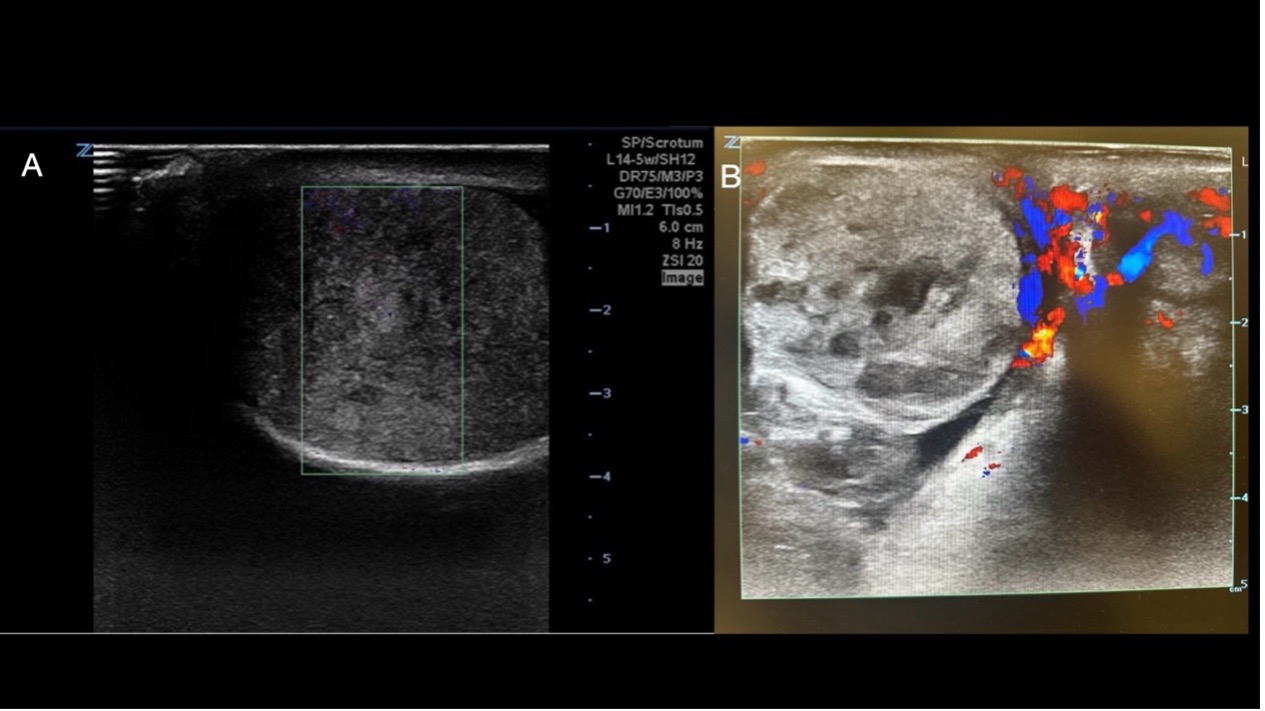
Absent testicular flow (Figure 8A)
Absence of doppler flow is highly predictive of TT, with 97% positive predictive value and 75% specificity for TT (7). If there is absence of flow, the case should be treated emergently as TT.
Decreased testicular flow (Figure 8B)
Early or partial testicular torsion (usually <360 degrees) may have preserved arterial flow since the arterial flow is impaired, but not completely obstructed. The color doppler signal may be decreased compared to the other side. Radiology ultrasound includes evaluation of arterial and venous waveform using spectral doppler to confirm this diagnosis.
Increased Blood Flow (Figure 8C)
In cases of torsion-detorsion, rebound reperfusion can result in hyperemia of the affected testicle. It may mimic the sonographic appearing of orchitis which may also have increased color flow. It is imperative to interpret increased perfusion in the clinical context.
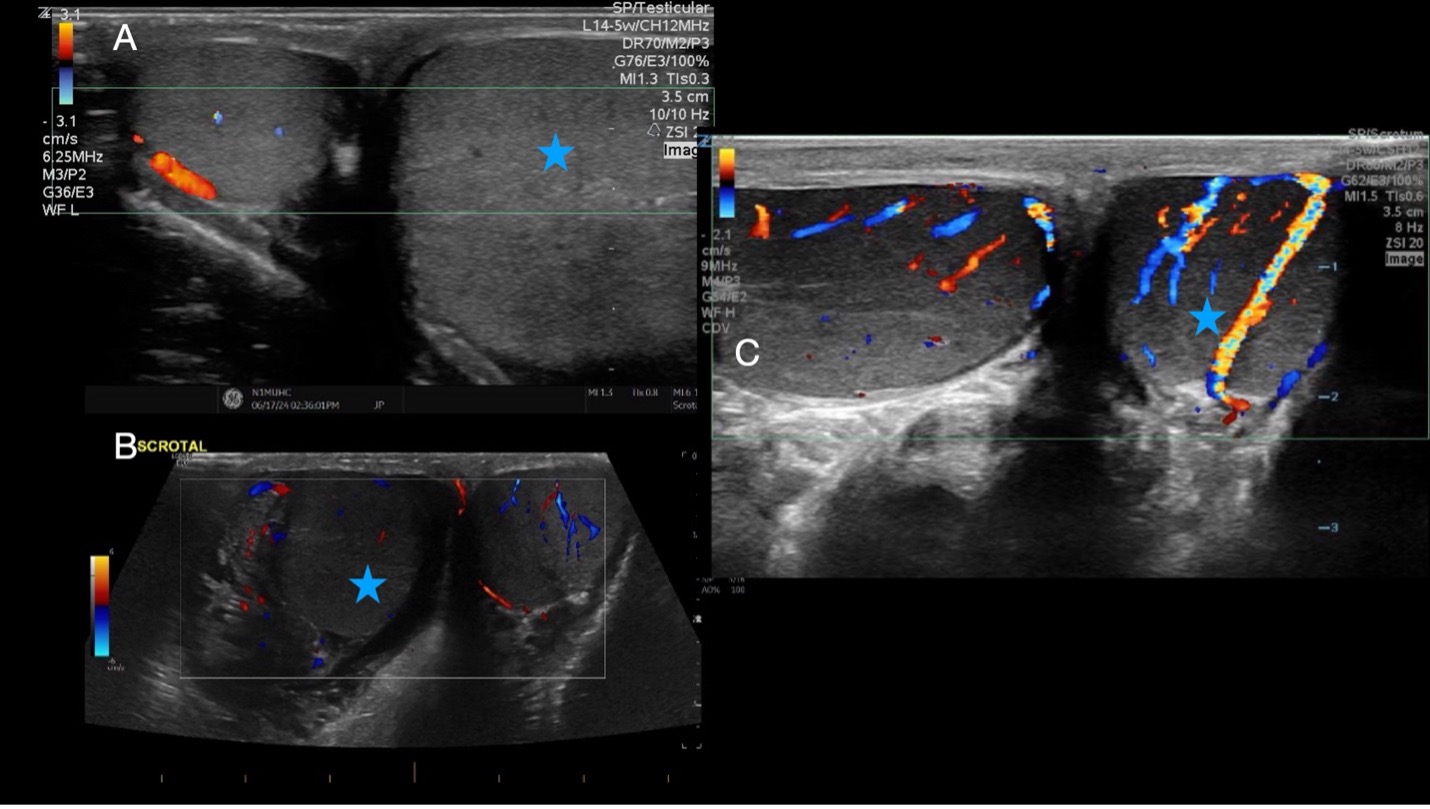
Figure 8. Abnormal testicular flow of the affected testicular (blue star) in the transverse plane A) Absent flow B) Decreased flow C) Increased flow on color doppler [15]
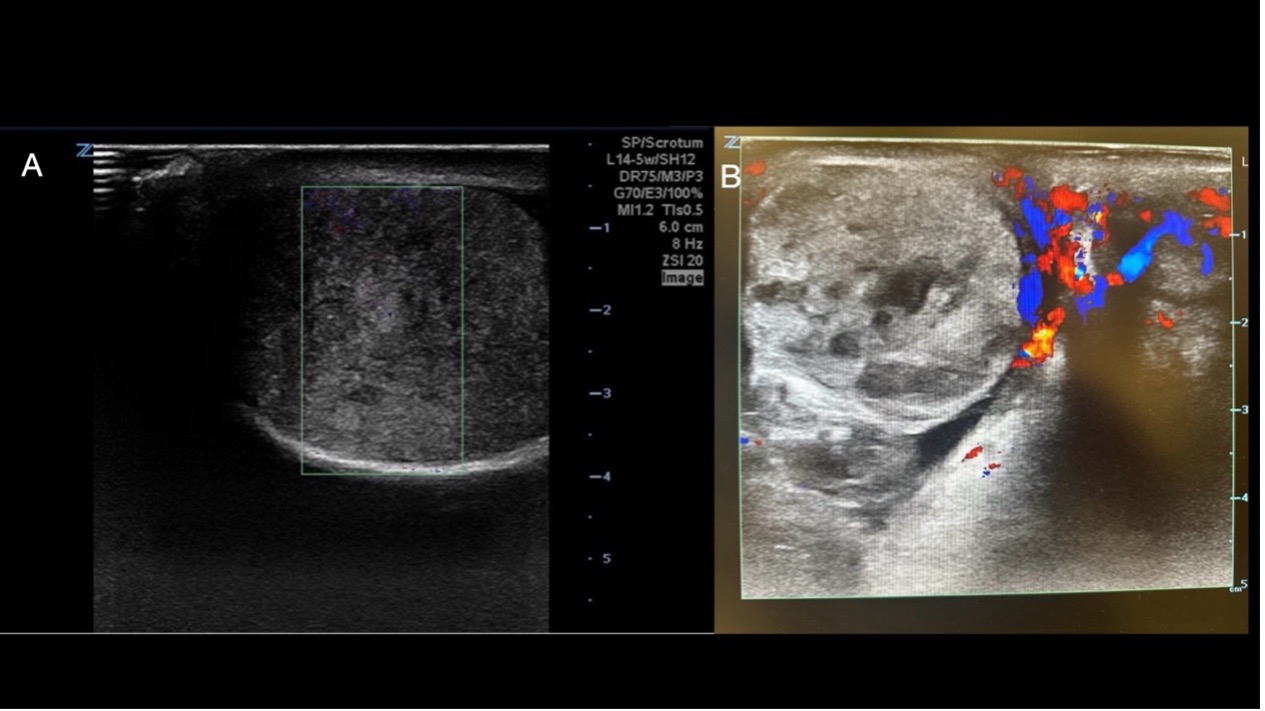
Figure 9. A) Heterogenous echogenicity of enlarged testicle and B) Heterogenous testicle with absent blood flow [15]
Video 2. Testicular torsion with absent flow and increased volume to left testicle
Spectral Doppler
Although not routinely used in PoCUS, spectral Doppler is commonly employed in Radiology when assessing for testicular torsion. Using spectral doppler in addition to color doppler to confirm torsion has been associated with a higher PPVs in predicting testicular torsion (7)
Pulsed wave spectral doppler can be used to confirm the presence of arterial and venous flow in the testicle in addition to color doppler since color doppler can be subject to motion artefact (16), but obtaining spectral waveforms can be difficult due to size of vessels and angle correction
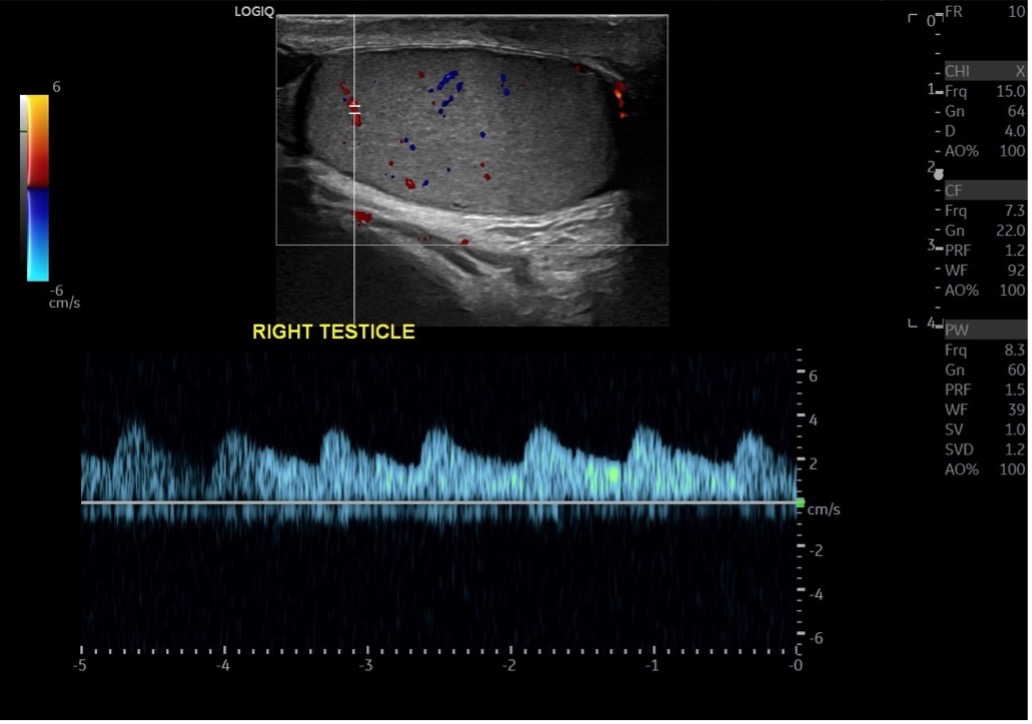
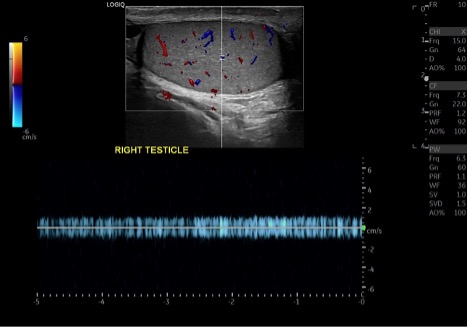
Normal Spectral Doppler:
With spectral doppler, arterial wave forms are pulsatile with distinct systolic and diastolic phases. Systolic phases begin with a sharp upstroke followed by a diastolic component that varies with resistance. Venous waveforms are continuous or monophasic (no systolic or diastolic peaks) and generally have lower velocity and some respiratory variation.
Normal arterial flow within the testicle will be pulsatile and exhibit high flow, low resistance, waveforms (16,17) (figure 10), whereas venous flow will exhibit low-velocity, continuous waveforms with minimal pulsatility (figure 11).
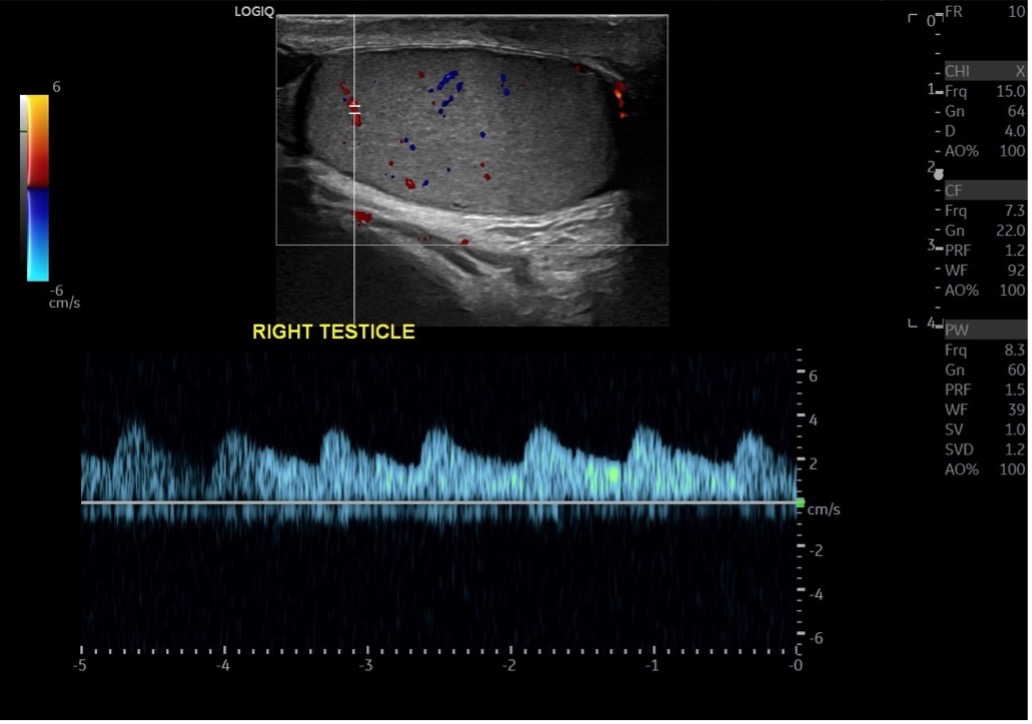
Figure 10: Arterial spectral doppler of the testicle
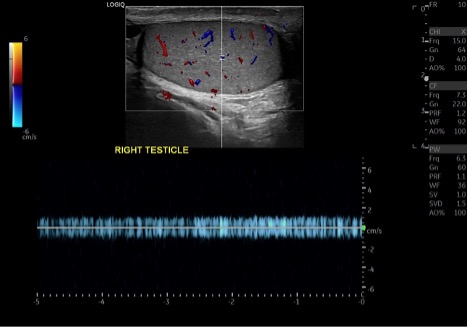
Figure 11: Venous testicular spectral doppler
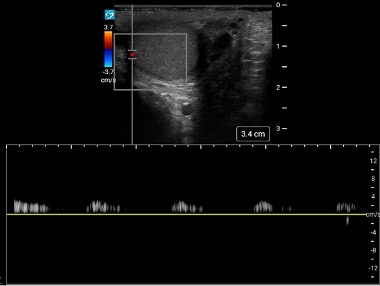
Abnormal Spectral Doppler: In early or complete torsion, the arterial waveforms will be absent or diminished. When comparing to the non-affected testicle, you may observe blunted waveforms with decreased flow velocity in the affected testicle and higher velocity flows in the non-affected testicle (16,17). Venous waveforms will be absent (17).
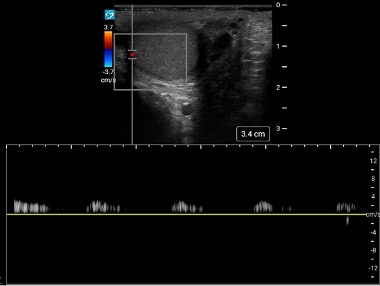
Figure 12: Torsed testicle with blunted arterial waveform. Image courtesy of Colin Bell, used with permission.
Secondary Findings:
Whirlpool Sign:The whirlpool sign is an US image of the spermatic cord above the testicle displaying a spiral with concentric circles. The finding is due to visualization of the twisted spermatic cord. A metanalysis looking at radiology performed US in patients over 3 months old with TT found a pooled sensitivity of 0.92 and pooled specificity of 0.99 for presence of whirlpool sign (18). The sensitivity of whirlpool sign is low in neonates < 30 days (18).
It’s important to note that this sign may not always be present. An important differential to consider is an epididymal abscess, although rare, can also present with a similar appearance.
Video 3. Whirlpool sign
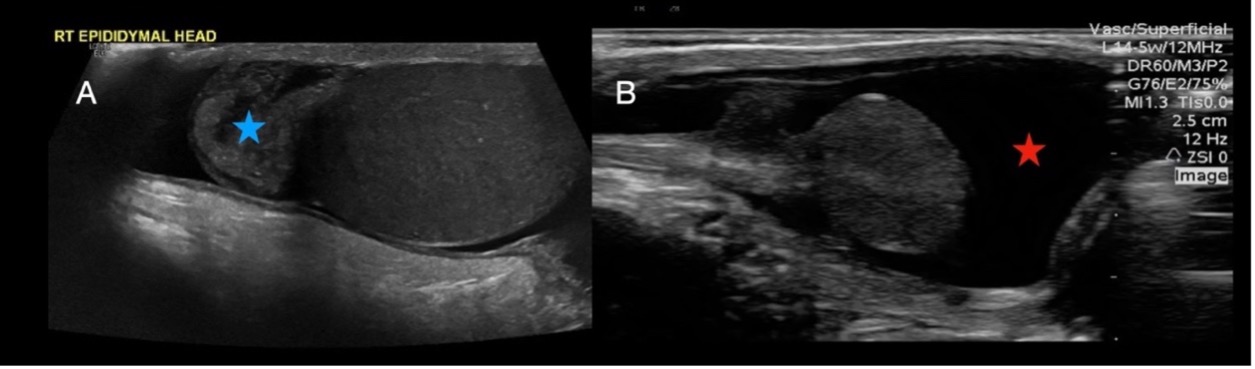
Epidydimal Swelling: (Figure 13A)
Secondary to the inflammatory process within the scrotum, the ipsilateral epidydimis may become swollen with testicular torsion.
Reactive Hydrocele: (Figure 13B)
Presence of hydrocele is nonspecific to testicular torsion but can be frequently encountered during ultrasound examination of the acute scrotum. The hydrocele fluid is anechoic and surrounds the testicle.
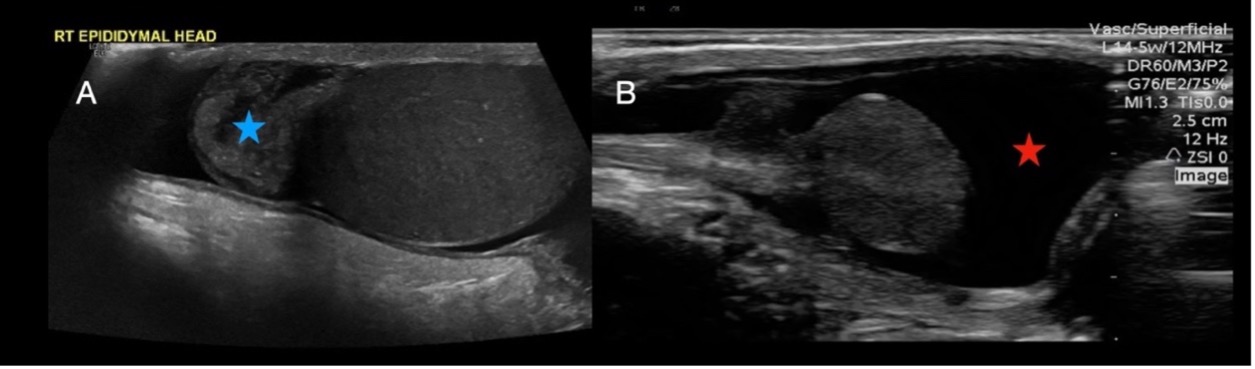
Figure 13. Testicular ultrasound in the longitudinal plane demonstrating A) enlarged epidydimal head (blue star) and reactive hydrocele (red star)