Anatomy Review: Where Am I Looking?
The veins of the forearm and the saphenous are the primary targets for ultrasound guided peripheral venous access. An ideal site involves choosing a vein that in less than 1.5 cm deep, 4mm in diameter and at least 1 cm in length [12]. The vessels of the distal upper arm are also considerations in those with difficult access, although can be more challenging to cannulate due to surrounding structures and deeper location [12]. If canulating the vessels of the upper arm the cephalic vein is preferred for its superficial location and distance from other structures. The basilic vein of the upper arm is the preferred site for PICC placement and should be avoided. The brachial veins lie very deep and in proximity to arteries and nerves which make access challenging. When using the vessels of the upper arm, consider placing a mid-length catheter as dislodgement of short catheters is more common at these sites.
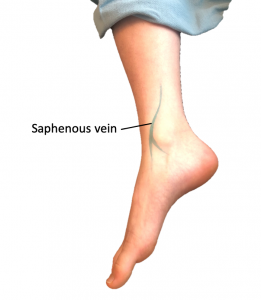
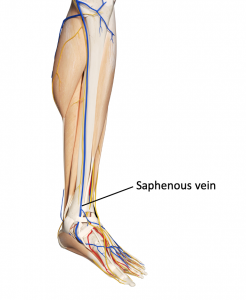
The cephalic vein begins at the anatomic snuff box and courses laterally along the forearm and upper arm, draining into the axillary vein (figures 1&2). The basilic vein drains the ulnar dorsal veins of the hand and courses medially up the forearm and upper arm, halfway up the forearm the basilic vein penetrates the brachial fascia and continues to run medial to the brachial artery (figures 1&2). Another site in the forearm includes the median antebrachial vein which courses the ventral aspect of the forearm between the cephalic and basilic veins before joining the basilic vein near the elbow (figures 1&2).
Figures 1&2: Upper extremity venous anatomy
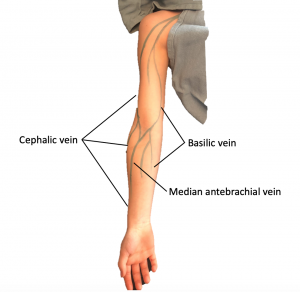
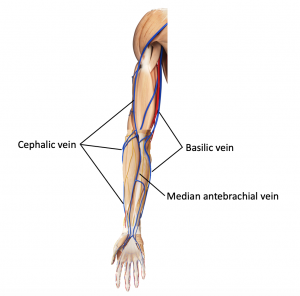
The saphenous originates anterior to the medial malleolus and ascends the medial aspect of the leg (figures 3&4).
Figures 3&4: Lower extremity venous anatomy