Subxiphoid IVC
The subxiphoid view visualizes the IVC as it enters the right atrium. The IVC appears as an anechoic, tubular, collapsible structure. Visually assessing the size and respiratory variation of the IVC may help estimate right atrial pressure and volume status, though this is not well correlated [21].
IVC diameter cutoff values are established for adults, however no such reference standards exist for the pediatric population. Some evidence supports the use of IVC-to-aortic ratios; however, these are unreliable and limited in practice. Therefore, a qualitative assessment focusing on IVC collapsibility and distensibility is recommended for pediatric RV strain assessment. And while the presence of collapsibility is reassuring, only the extremes (marked collapse or minimal/no collapse) are truly informative in 2D assessment of the pediatric population.
Assessment should be made in the long axis with the IVC displayed horizontally.
What is Normal?
- Small caliber
- Highly collapsible
** In children receiving positive pressure ventilation (PPV), the IVC behaves differently than in spontaneous breathing: its diameter expands during inspiration and contracts during expiration [22]. It is important to consider this when assessing the IVC in children receiving PPV.
Figure 20: Subxiphoid IVC view in cardiology convention demonstrating normal diameter and respiratory variation.
What is NOT Normal?
- A plethoric IVC with little to no respiration
· In these cases, it is important to question why the IVC appears distended with minimal variation (e.g., RV strain, tamponade).
- Flat/nearly collapsed
· May suggest hypovolemia or distributive states; fluid administration might be warranted, but always interpret in the context of the overall clinical picture.
Practice Pearl:
Intermediate appearances, where the IVC is neither flat, highly collapsable or plethoric, are unreliable and challenging to interpret in pediatric populations. The extremes (marked collapse or minimal/no collapse) are the findings that are informative. Always prioritize the clinical context over IVC PoCUS findings alone.
Figure 21: Subxiphoid IVC view cardiology convention demonstrating plethoric IVC with little to no collapse with respiratory variation.
M-Mode of the IVC
Mmode can be applied to the IVC to help visualize and quantify respiratory variation.
> The standard assessment point is just caudal to the hepatic vein confluence [23].
> On M-mode, the IVC will appear as a thin, anechoic band which will change in diameter over the respiratory cycle, creating a wavelike pattern that reflects the vessel’s dynamic collapse and distension (figure 22).
A key limitation to be aware of on assessment of the IVC is that the IVC moves in both craniocaudal and mediolateral directions during respiration. These movements can introduce error as this displacement cannot always be detected in longitudinal 2D or Mmode. This can potentially lead to underestimating IVC caliber and overestimation of collapsibility and distensibility (figure 23) [23].
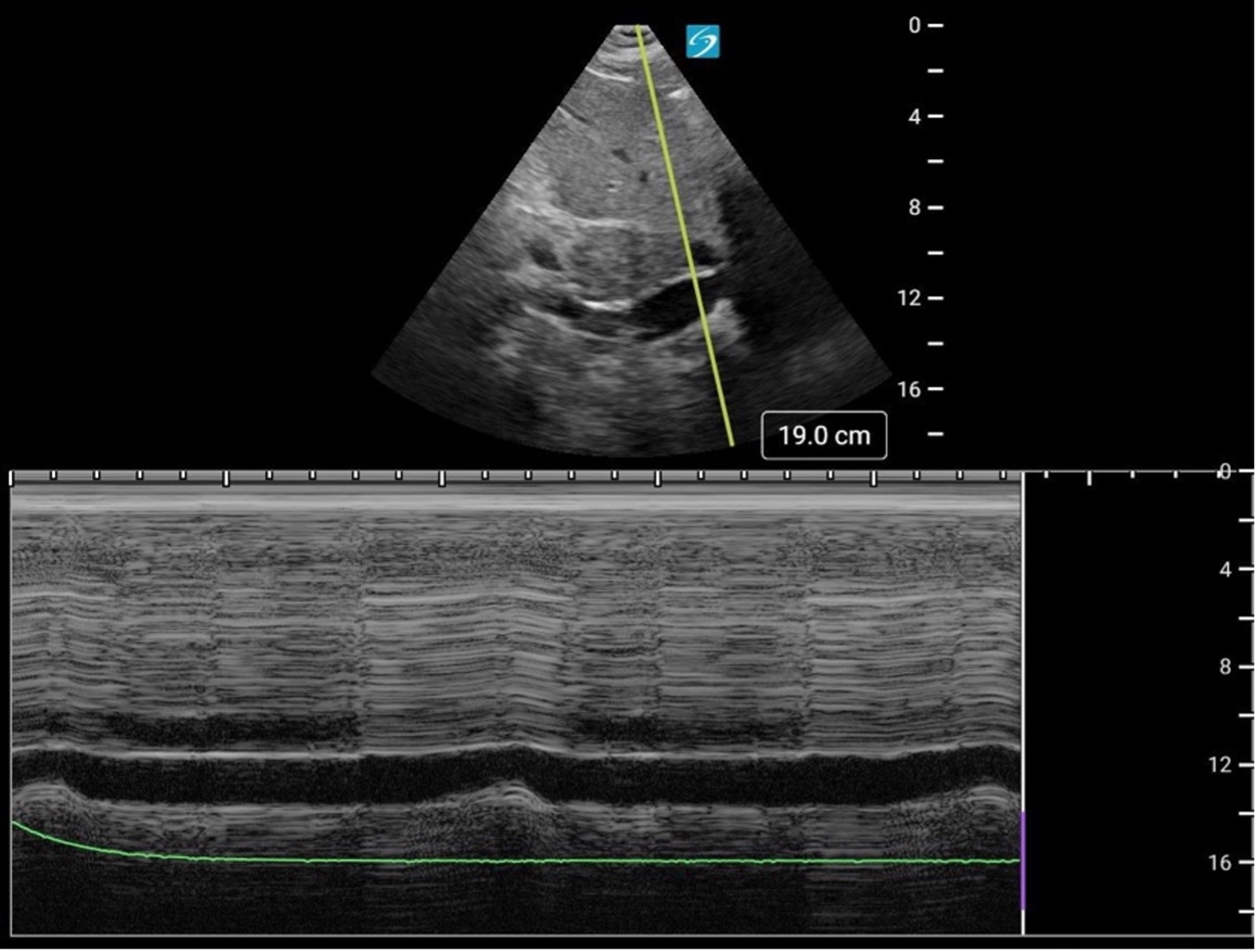
Figure 22. Mmode of the IVC from the subxiphoid position.
Figure 23. Subxiphoid Mmode of the IVC demonstrating lateral displacement, falsely suggesting IVC collapse.
Advanced Practice Pearl: Color Doppler of the Hepatic veins
Hepatic vein Doppler assessment on PoCUS can provide indirect evidence of RV strain. This represents an advanced PoCUS skill and will be covered in a future KidSONO advanced practice module.
