Author: Melanie Willimann
Secondary Author: Mark Bromley
Reviewers: Amanda Toney, Paul McKenna
**To continue through the course, make sure to select the “Mark as Completed” button below, and at the end of each lesson page that follows.
Introduction
The most common initial test for respiratory distress is chest x-ray. Recently, growing evidence has shown that PoCUS can reliably detect thoracic pathology with equal if not better sensitivity than chest x-ray (CXR). In the case of pleural effusions, ultrasound is both more sensitive and specific than CXR. It has the advantage of differentiating causes of “white out” on CXR given its ability to characterize effusion and other pathology. It is also useful in guiding diagnostic and therapeutic procedures. Computed tomography, which offers little advantage over US is impractical and comes with the cost of significant radiation.
Why Ultrasound?
Traditionally it was thought that ultrasound was not a useful modality for investigating lung pathology because air scatters ultrasound waves. There has been a growing body of evidence in recent years contradicting this practice. Given that the fluid accumulated in the pleural space transmits ultrasound waves, pleural effusions can easily be detected by ultrasound.
A recent meta-analysis looking at the test characteristics of PoCUS for pleural effusion in trained users found a sensitivity of 93% and specificity of 96% when compared to either CT or fluid on aspiration [1]. This is significantly superior to CXR that has a sensitivity of 20-75% and a specificity of 50-90% [2]. Therefore, ultrasound is therefore the first-line imaging choice in investigating pleural collections [3,4,5,6].
Implementation of lung ultrasound has been shown to decrease the number of chest x-rays and CT scans performed in the ICU. In the emergency department, it has been shown to decrease the length of stay compared to patients who underwent chest radiography [7,8].
PoCUS is safe, timely and effective for the diagnosis of pleural effusion.
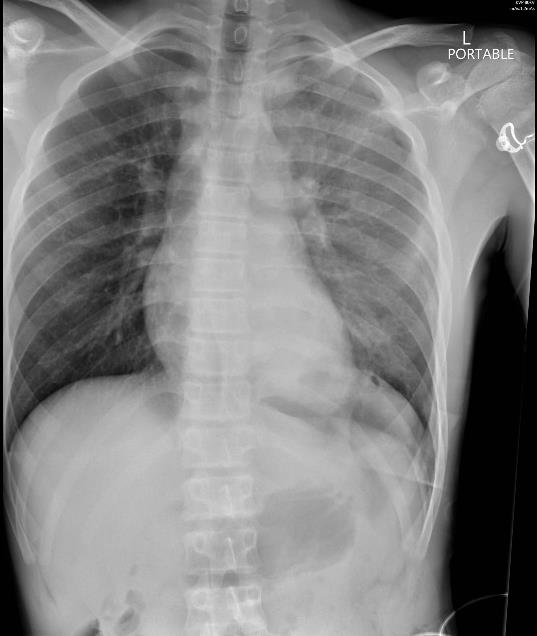 Figure 1. Supine CXR: Hemothorax
Figure 1. Supine CXR: Hemothorax PoCUS:
Sensitivity 93%
Specificity 96%
CXR:
Sensitivity 20-75%
Specificity 50-90%
PoCUS vs CXR in trained users [1]

