What is NOT normal
Reactive Lymph Node
Usually due to a benign, reversible enlargement of nodes in response to antigenic stimulus. In the pediatric population, the etiology usually is secondary to viral or bacterial pathogens. Viral infections are the most common cause of reactive adenopathy.(9) Lymph node involvement may be acute or chronic, localized or generalized.
Size: Reactive lymph nodes are usually larger than normal lymph nodes.
Shape: Reactive nodes maintain their normal ovoid shape, except in the submandibular region where they are usually round.
Echogenicity: Primarily homogenous.
Internal structure: Persevered normal node architecture, with a hypoechoic cortex and a hyperechoic medulla, and fatty central hilum.
Surrounding tissue: Typically, no or limited inflammatory changes in the surrounding tissues of normal or reactive lymph nodes
Vascularity: Color Doppler imaging reveals more prominent vessels at the hilum. Hilar vascularity may be pronounced, with vessels extending from the hilum to the periphery of the node.
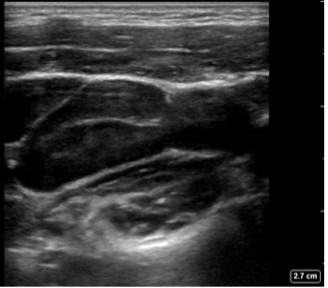
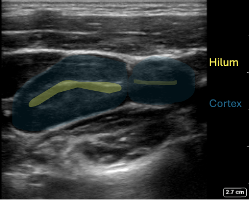
Figure 5. Reactive Lymph nodes in a longitudinal plane: Enlarged oval shaped node, expected echotexture with a hypoechoic cortex and more echogenic central hilum. Note the absence of hyperechoic fat surrounding the node
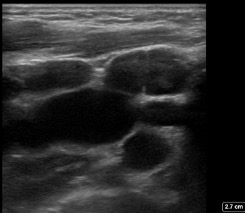
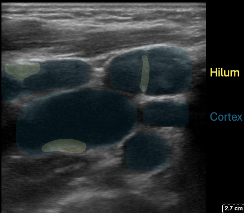
Figure 6: In the transverse plane multiple oval shaped nodes with the expected echogenicity
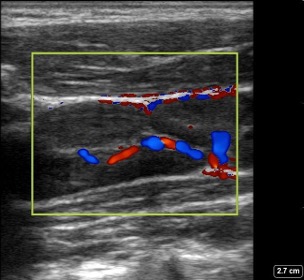
Figure 7: Reactive Lymph node in a longitudinal plane with color Doppler: shows increased hilar vascularity.
Suppurative Lymphadenitis
Suppurative lymphadenitis is caused by an infection of one or more nodes. The most common pathogens are Staphylococcus aureus and group A streptococcus (GAS). This might occur following reactive lymphadenopathy with opportunistic infection by bacteria found typically in the ear, nose, throat, and on the skin. Infections that occur after dental or oral surgeries are more typically polymicrobial, with anaerobic bacteria more frequent (9).
Size: Typically enlarged node or confluence of nodes. Usually 1-4 cm in greatest dimension.
Shape: Ovoid to round.
Echogenicity: Heterogenous with areas of decreased and increased echogenicity.
Internal structure: The node appears hypoechoic with irregular wall thickness but preserved wall margin. The central hilar stripe is not visible. Internal hyperechoic areas are present, indicating the presence of purulent material and debris.
Surrounding tissue: Thickening can be observed in the surrounding tissues and subcutaneous layers. Often posterior acoustic enhancement is present.
Vascularity: Central avascularity, often with increased vascularity to the nodal periphery and to the inflamed surrounding soft tissues.
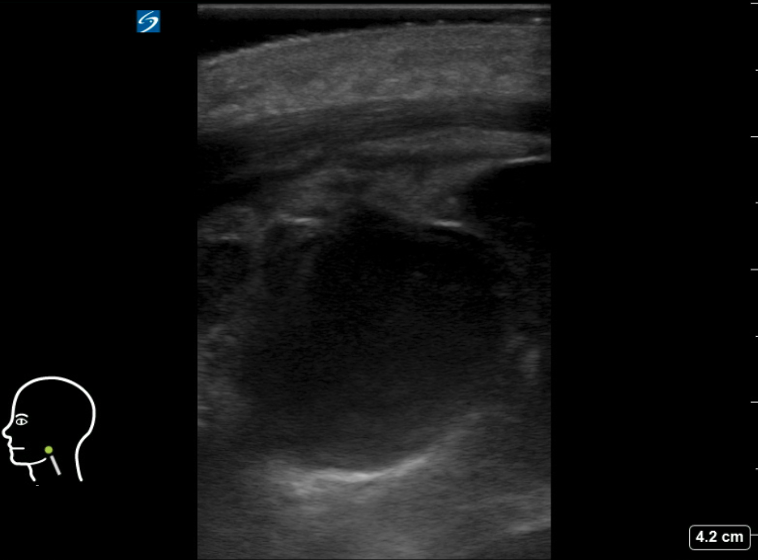
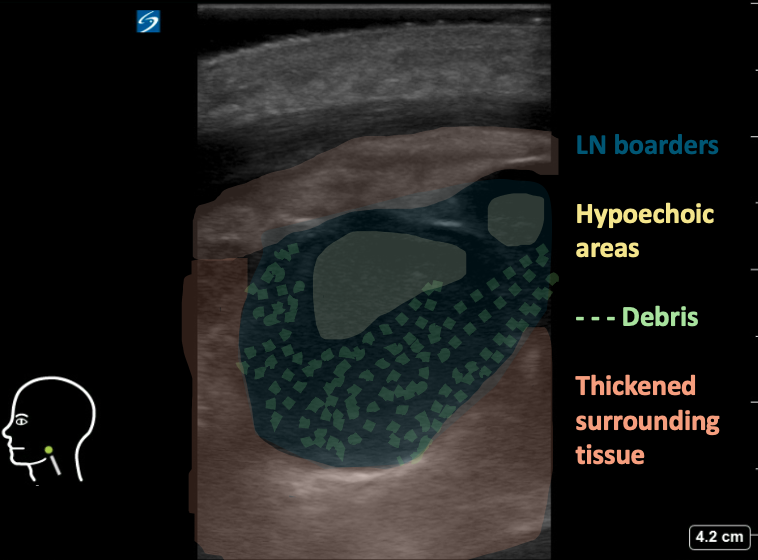
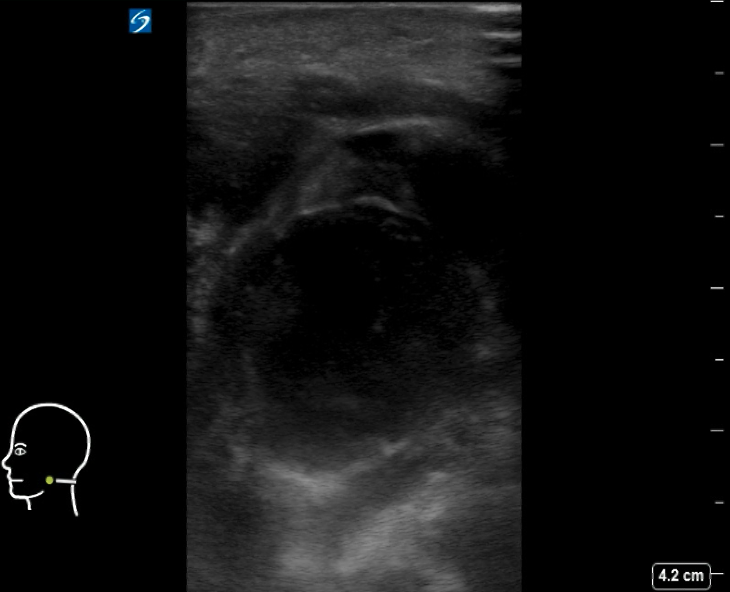
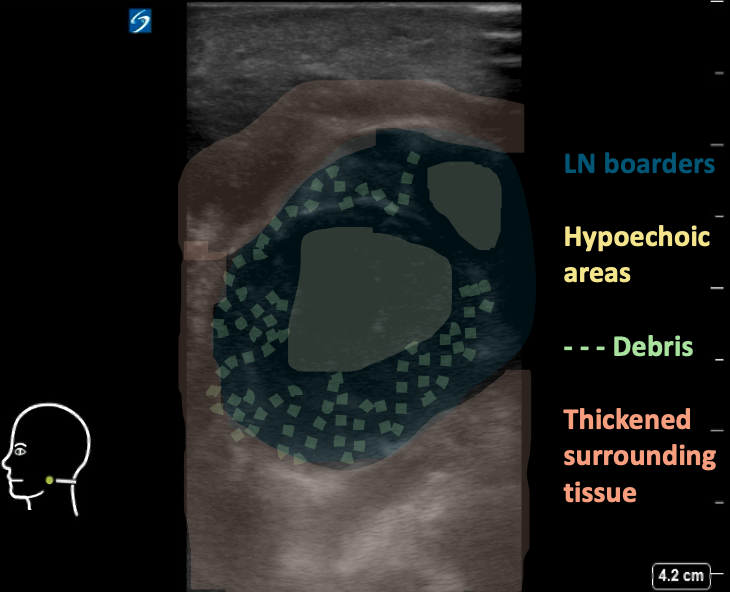
Figure 8AB: Suppurative cervical lymph node, in the longitudinal (A) and transverse (B) planes. Enlarged and round in both views, with loss of normal hilar architecture and heterogeneous echotexture including hypoechoic areas and peripheral debris. Note the thickening of the surrounding tissue.
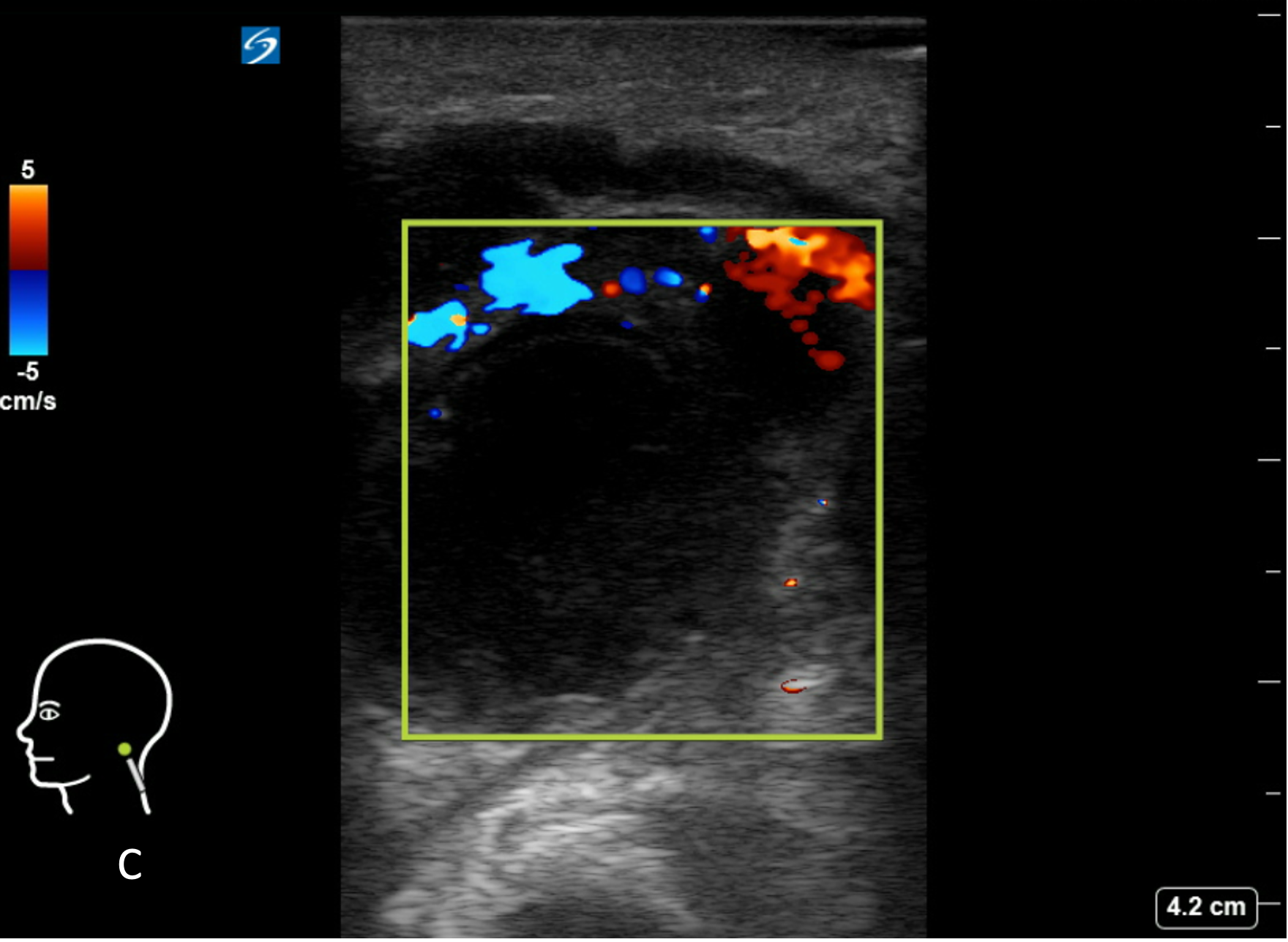
Figure 8C: Corresponding image with color Doppler. Central avascularity.
Abscess formation:
Suppurative lymphadenitis may progress and form an abscess.
Size: Usually 1-4 cm in greatest dimension, but might grow to a large size as well
Shape: Usually irregular shape and margins.
Echogenicity: Complex, heterogeneous, with hypoechoic or anechoic center.
Internal structure: Loss of normal nodal architecture, and heterogeneous echogenicity. Overall hypoechoic lymph node with internal hyperechoic areas, presenting purulent material and debris. Internal septations are also common. The presence of intensely echogenic, mobile spots with “dirty” shadowing strongly suggests the presence of air/gas bubbles.
Surrounding tissue: Thickening of both the tissue and subcutaneous layers in surrounding tissue. Fluid or edema within the subcutaneous layers is common, with hypoechoic strands of edema fluid,creating a “cobblestone” appearance.
Vascularity: Central avascularity, often with Increased vascularity to both the node periphery and surrounding inflamed soft tissues.

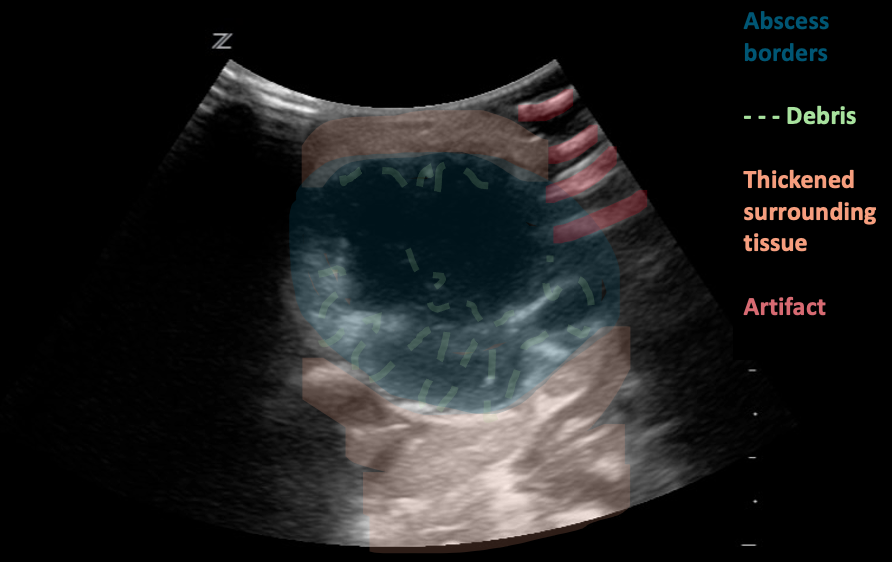
Figure 8: Neck abscess, transverse plane. Irregular shape and margins with anechoic regions and hyperechoic debris (likely purulent material). Edema and thickening of the surrounding tissues. Images courtesy of EDSonoShare, licensed under CC BY-NC-SA
Figure 9: Neck abscess, transverse plane. Irregular shape and margins with anechoic regions and hyperechoic debris (likely purulent material). Edema and thickening of the surrounding tissues. Video courtesy of EDSonoShare, licensed under CC BY-NC-SA
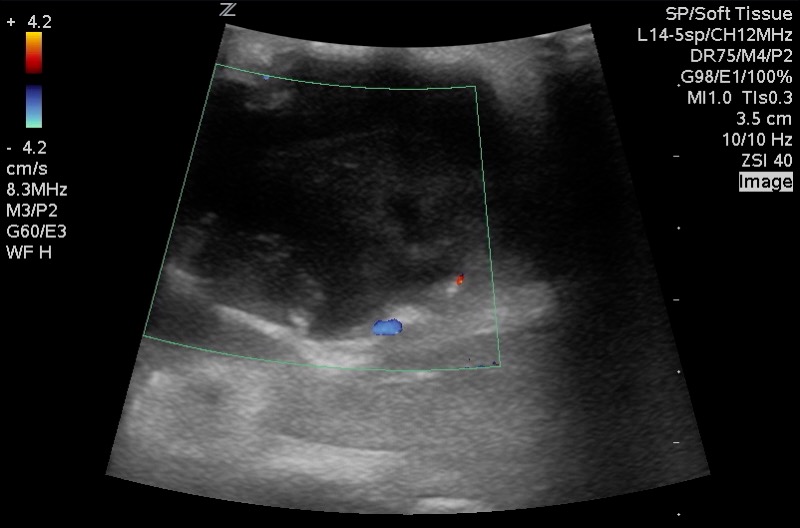
Figure 10: Corresponding image with Color Doppler. Central avascularity with increased peripheral flow. Images courtesy of EDSonoShare, licensed under CC BY-NC-SA
Lymphomatous nodes:
Lymph nodes can be affected by either Hodgkin’s or non-Hodgkin’s lymphoma. On its own, sonography cannot differentiate between these two types of lymphoma.
Size: Lymphomatous nodes typically exceed 10 mm in size in the transverse plane. Cervical node diameter alone is unreliable for distinguishing lymphomatous nodes from normal or from other pathological causes of node enlargement.
Shape: Usually round to elliptical and well-defined
Echogenicity: Homogenous or slightly heterogenous.
Internal structure: The nodes appear solid and hypoechoic in comparison to nearby muscle. The internal structure frequently displays intranodal reticulation or micronodular patterns. The echogenic hilum is often not present.
Surrounding tissue: Generally, does not show signs of inflammation (i.e. increased echogenicity). These nodes may display posterior acoustic enhancement.
Vascularity Most typically exhibit a mixed vasculature, including both hilar and peripheral vessels. Isolated peripheral vascularity is uncommon in lymphomatous nodes.
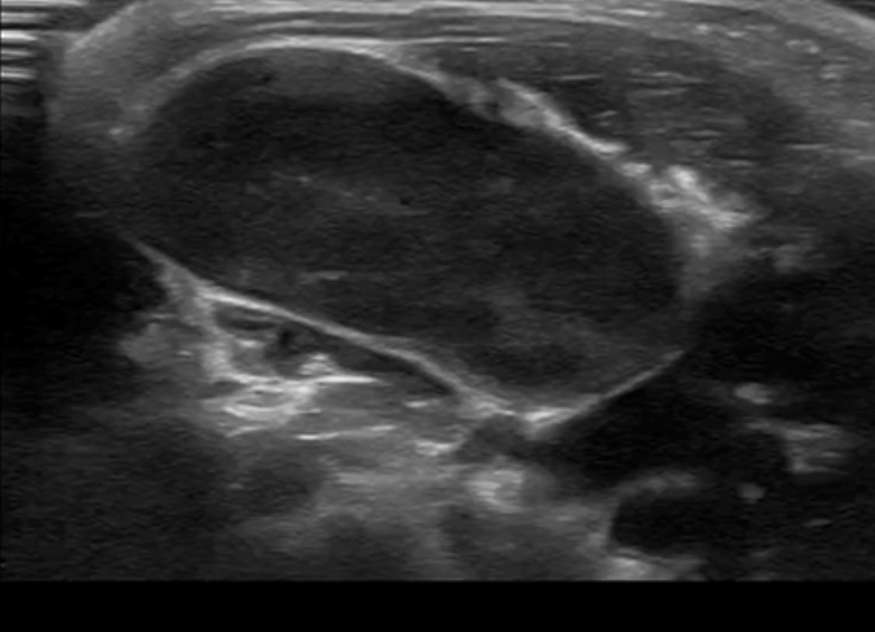
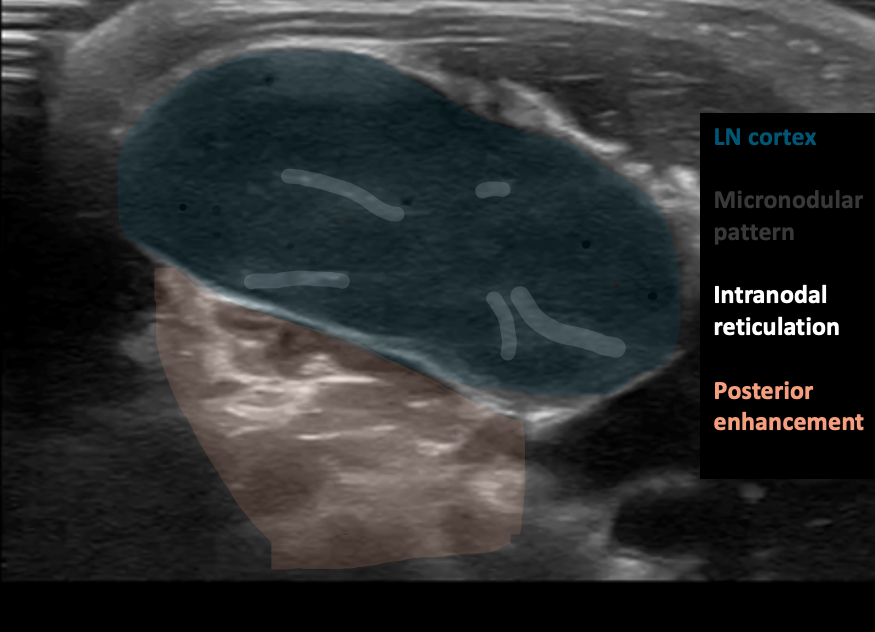
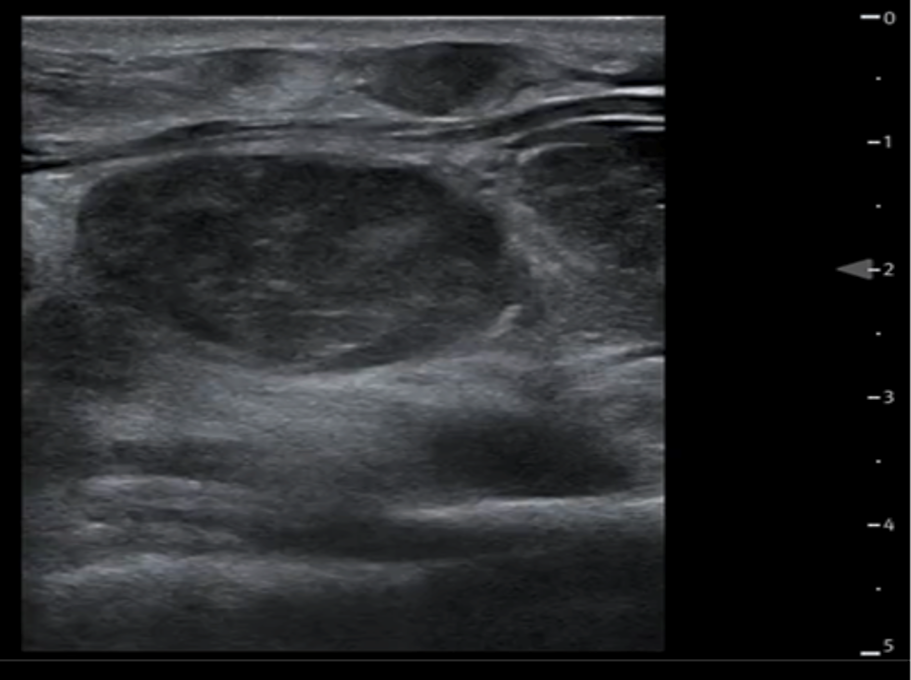
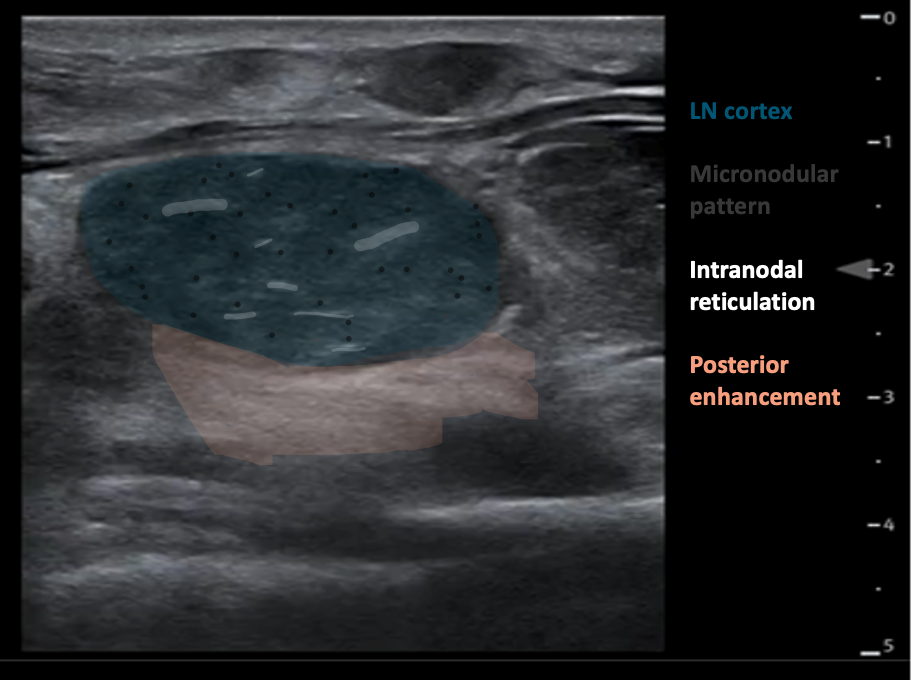
Figure 11AB: Lymphomatous node, in the longitudinal (A) and transverse (B) planes. Well-defined, solid, and hypoechoic, with a micronodular architecture and posterior acoustic enhancement. [Images courtesy of the SickKids de-identified image bank]
