Anatomy of the Inguinal Crease
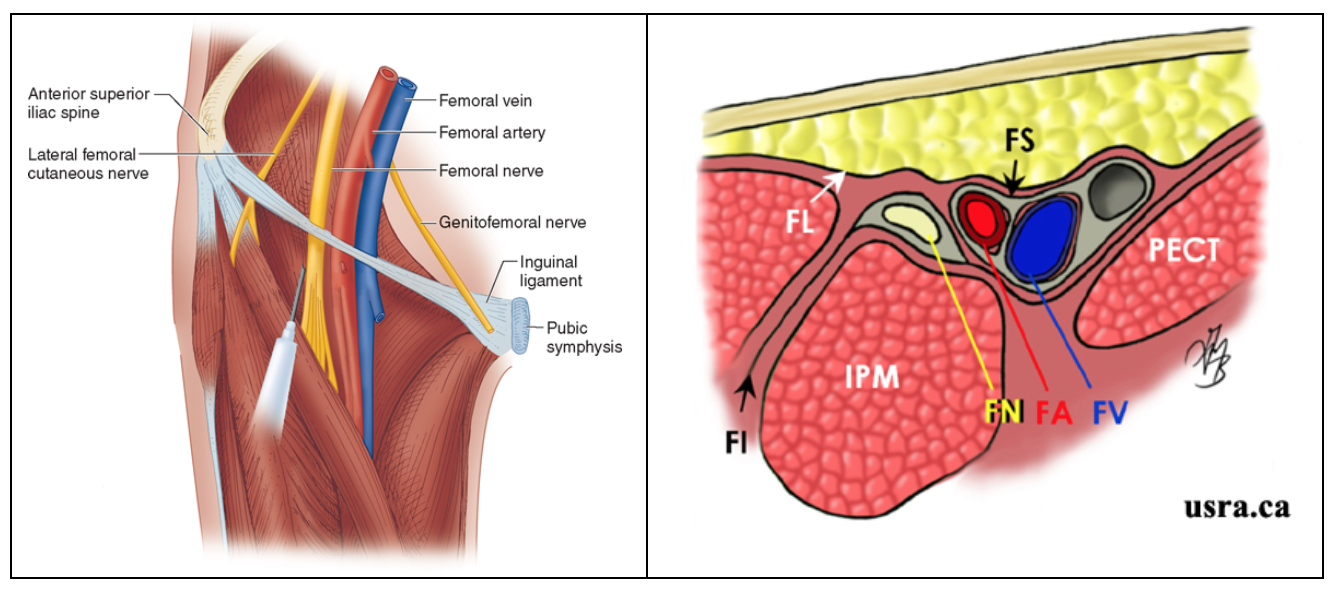
Prior to placing the ultrasound probe on the patient, it is important to understand the cross-sectional anatomy at the level of the inguinal crease. Most superficially you will find the skin and subcutaneous tissue. Immediately deep to this lies the fibrous membrane of the fascia lata. Deep to the fascia lata, lies the femoral nerve, artery and vein (from lateral to medial). Of note, medially the femoral artery and vein are surrounded by the thick femoral sheath while laterally the femoral nerve is surrounded by the fascia iliaca. Deep to the neurovascular bundle you will identify the psoas and pectineus muscle, again from lateral to medial (figure 4).
Figure 4: Anatomy of the Inguinal Crease
Sonographic Anatomy
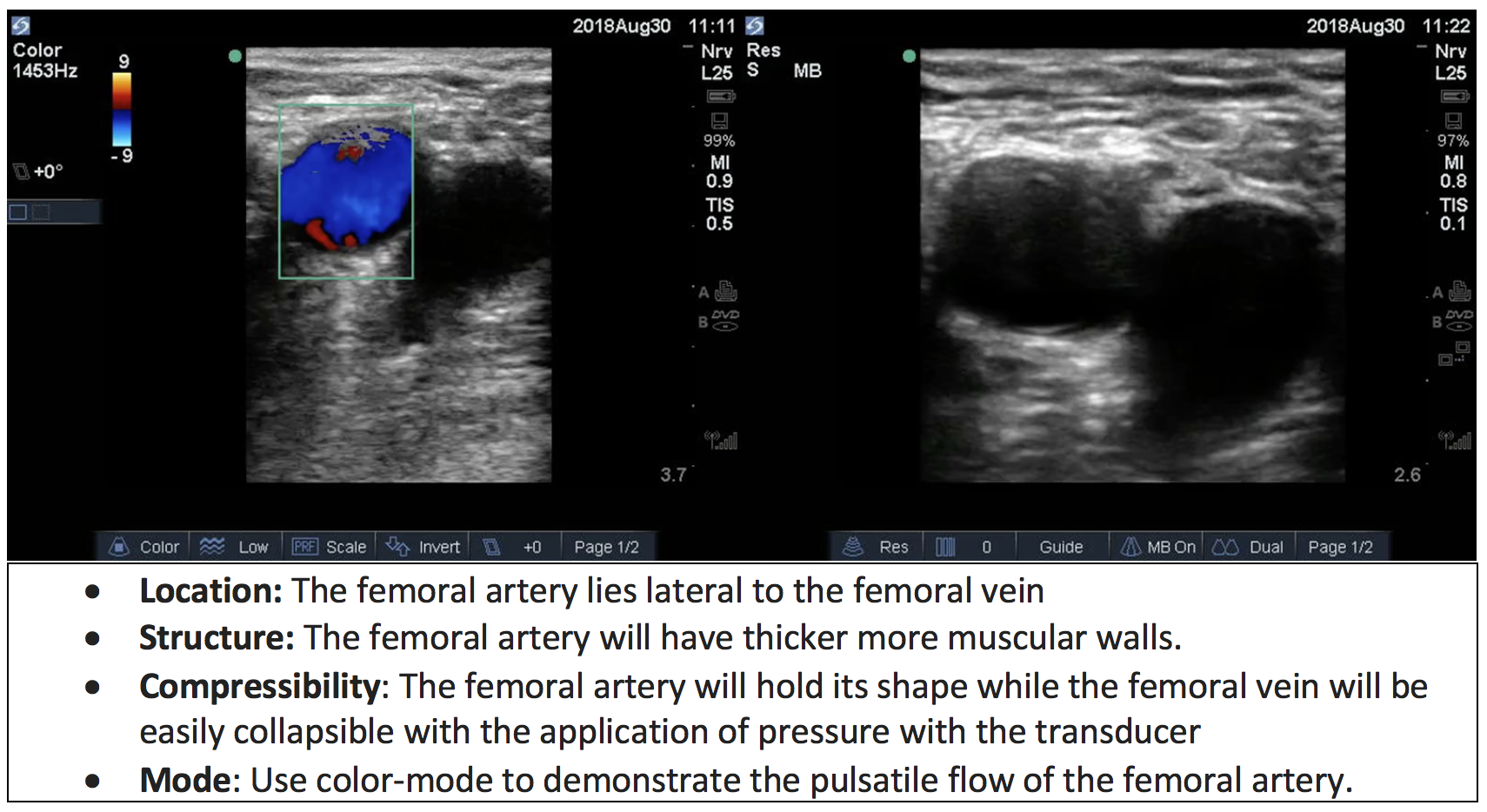
The ultrasound transducer is first placed along the inguinal crease directly above where the femoral artery is palpated. First, identify the femoral artery and vein. Both will appear as hypoechoic (dark) structures, but the femoral artery will also be non-compressible and pulsatile. Remember, the femoral vein lies medial to the artery and will collapse when pressure is applied with the ultrasound transducer, if you cannot see the vein reduce the pressure you are applying with the transducer until the vein appears medial to the artery (figure 7).
Figure 5: Differentiating the femoral artery from the femoral vein.
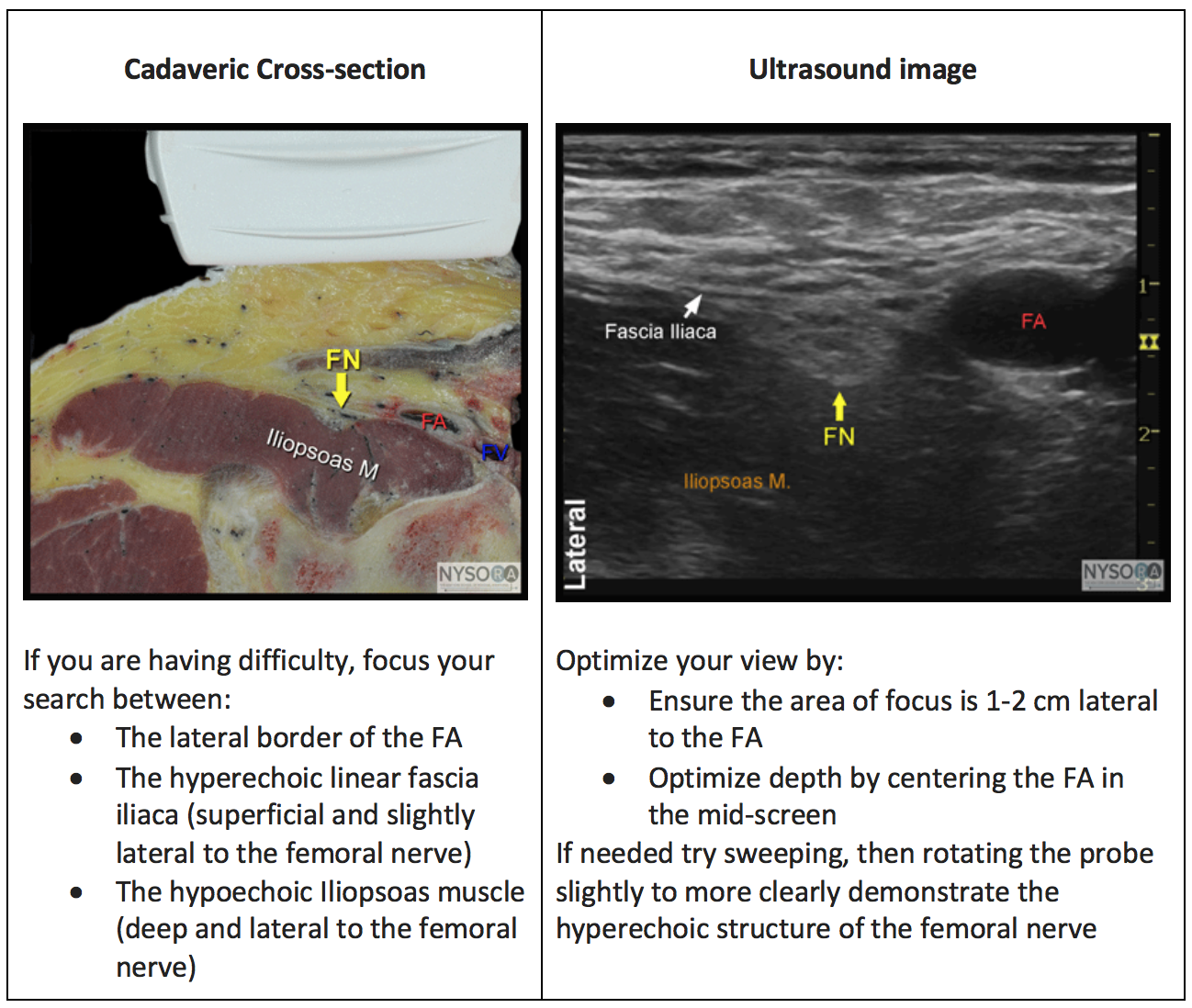
The femoral nerve lies lateral to the femoral sheath which contains the femoral artery, and femoral vein (figure 6) and is covered by the hyperechoic linear plane of the fascia iliaca. The femoral nerve is typically immediately superficial to the hypoechoic iliopsoas muscle (7, 8). The femoral nerve has a hyperechoic appearance on ultrasound and can vary between a circular, triangular and flat appearance (Video 1).
Video 1: Sono-anatomy of the inguinal crease
In some patients you may see the deep inguinal lymph nodes lying medial to the femoral vein. Lymph nodes appear as slightly hyperechoic circular structures which can easily be confused with the femoral nerve. However, they will be located much more medially than the femoral nerve, and they will disappear from the screen as the ultrasound probe is translated from caudad to cephalad along the skin.
Sometimes the femoral nerve can be difficult to identify, remember it is found lateral to the femoral artery, superficial to the iliopsoas muscle and deep to the fascia iliaca. It has a hyperechoic appearance on ultrasound and can vary between a circular, triangular and flat appearance (figure 6).
Figure 6: Localizing the femoral nerve