Introduction
Acute appendicitis is a common surgical emergency among children and adolescents, affecting tens of millions of patients globally each year, with the highest incidence occurring between ages 10 and 19 [1,2]. Prior to the advent of medical imaging and modern surgical techniques, it accounted for significant morbidity and mortality [3]. In the modern era in North America death secondary to acute appendicitis and its complications have become rare, with decreased incidence, improved diagnosis, increased treatment options, and availability of prompt surgical management all playing a role in the improvement in outcomes [4]. Diagnosis of appendicitis typically involves a combination of clinical evaluation and medical imaging, which plays a central role in confirming the diagnosis and guiding management. While history and physical examination remain important, most major centers rely on imaging before proceeding to surgery, especially in cases with equivocal presentations. Scoring systems may also be used to support decision-making and determine the need for imaging [5,6]
Why Ultrasound?
Ultrasound is a valuable diagnostic tool in cases of suspected appendicitis, particularly in children and pregnant populations, where minimizing radiation exposure is paramount. It is a non-invasive modality and does not require complete stillness, making it particularly suitable for younger children or those who may have difficulty remaining still for cross-sectional imaging such as CT or MRI.
Ultrasound has high sensitivity in detecting inflammation and structural abnormalities in the appendix, allowing for dynamic assessment of the appendix and surrounding tissues [7]. It also offers sufficient specificity to aid in distinguishing between uncomplicated and complicated appendicitis [7]. Its diagnostic performance can vary depending on factors such as operator experience and patient characteristics, including body habitus, difficulty tolerating probe pressure, and the presence of bowel gas, among others. Despite this variability, ultrasound for the diagnosis of acute appendicitis in pediatric patients by radiology (RADUS) has demonstrated a sensitivity of 97.1% and specificity of 94.8%, and when nondiagnostic studies are excluded, these values increase to 98.8% and 98.3%, respectively [7].
There is, however, high variability in the sensitivity and specificity reported across the publications included in all three analyses [8-10], but overall, the data supports PoCUS as a valuable tool for diagnosing acute appendicitis, particularly in pediatric patients.
Additionally, PoCUS for appendicitis allows real-time imaging, and can be readily performed at the bedside, facilitating prompt diagnosis and timely initiation of appropriate treatment, thereby reducing the risk of complications associated with appendicitis. Studies have shown that ED PoCUS can significantly reduce pediatric ED length of stay when performed by both fellowship and non-fellowship PoCUS trained emergency physicians [11,12] and reduce CT usage [11].
Considering these advantages, it is important to recognize that PoCUS for appendicitis should be viewed as a useful diagnostic tool, with its strengths in real-time imaging and immediate assessment. However, due to the prevalence of non-diagnostic exams, it is most effective when used as a rule-in test, where a positive result supports the diagnosis—helping guide immediate management decisions, but a negative scan alone does not reliably rule it out.
Table 1: Summary chart of Sensitivity and Specificity values for diagnosing appendicitis in pediatric populations
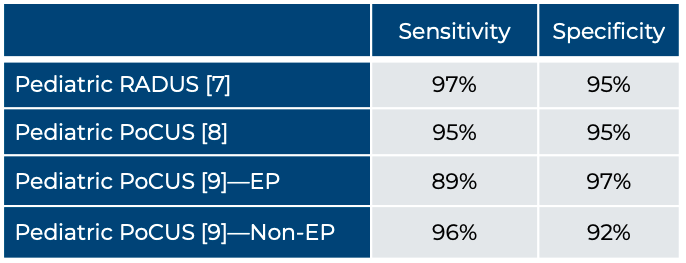
*CI = 95%. EP = Emergency physician
